Analysis of gut microbiota in patients with nonalcoholic steatohepatitis with different Traditional Chinese Medicine syndrome type
-
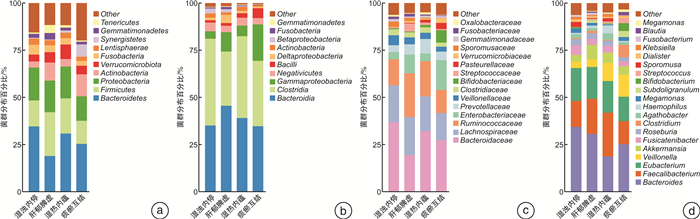
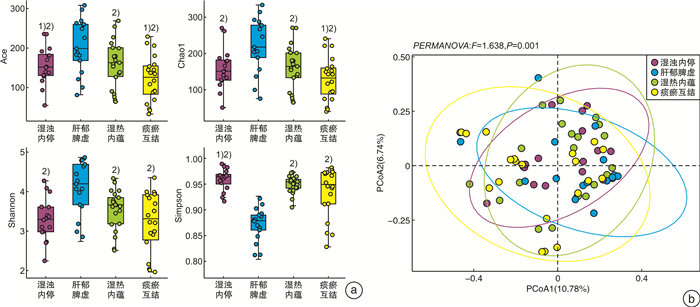
摘要: 目的 探讨不同中医证型非酒精性脂肪性肝炎(NASH)患者肠道菌群的差异。方法 选择符合诊断和纳入标准的NASH患者74例,其中湿浊内停证21例、肝郁脾虚证16例、湿热内蕴证17例和痰瘀互结证20例。分别收集各组患者血清生化指标和肝脏硬度与可控衰减参数,采用16S rRNA高通量测序检测各组患者肠道菌群的差异性。结果 各中医证型NASH患者的肝功能指标[天门冬氨酸氨基转移酶(AST)、丙氨酸氨基转移酶(ALT)、γ-谷氨酰基转移酶(GGT)]、血脂[总胆固醇(TC)、甘油三酯(TG)]、肝纤维化指标(透明质酸、层粘连蛋白、Ⅲ型前胶原蛋白和Ⅳ型胶原)、可控衰减参数(CAP)和肝脏硬度测量值(LSM)的比较,差异均有统计学意义(P<0.05),而碱性磷酸酶(ALP)、高密度脂蛋白胆固醇(HDL-C)和低密度脂蛋白胆固醇(LDL-C)的比较,差异均无统计学意义(P>0.05)。α多样性结果显示,与肝郁脾虚证比较,湿浊内停证、湿热内蕴证和痰瘀互结证Ace、Chao1和Shannon指数均明显降低,Simpson指数均明显升高(P<0.05)。与湿热内蕴证比较,湿浊内停证和痰瘀互结证Ace和Chao1指数均明显降低,Simpson指数均明显升高(P<0.05)。各中医证型特征菌属鉴定结果显示,湿浊内停证肠道菌群中Ruminococcus和Dorea菌属的丰度明显增加;肝郁脾虚证肠道菌群中Oscillospira和Akkermansia菌属的丰度明显增加;湿热内蕴证肠道菌群中Heamophilus和Agathobacter菌属的丰度明显增加;痰瘀互结证肠道菌群中Alistipes菌属的丰度明显降低,Streptococcus菌属的丰度明显增加。结论 各中医证型肠道菌群多样性和菌群结构存在差异,可能参与NASH病情和中医证候的发生与发展。Abstract: Objective To analysis the difference of gut microbiota in patients with nonalcoholic steatohepatitis(NASH) with different Traditional Chinese Medicine(TCM) syndromes type.Methods Seventy-four patients with NASH met the criteria were selected, including 21 cases of congestion of dampness turbidity, 16 cases of liver depression and spleen deficiency, 17 cases of accumulation of dampness and heat, and 20 cases of phlegm and blood stasis. Serum biochemical indexes, CAP and LSM of patients in each group were collected, and gut microbiota of NASH patients with different TCM syndromes were also analysis by 16S rRNA high-throughput sequencing.Results There were statistically significant differences in liver function indexes(AST, ALT and GGT), lipids indexes(TG and TC), liver fibrosis indexes(HA, LN, PⅢNP and CⅣ), CAP and LSM of NASH patients with different TCM syndrome types(P<0.05), while there was no statistically significant difference in ALP, HDL-C and LDL-C(P>0.05). The diversity results showed that Ace, Chao1 and Shannon indexes of congestion of dampness turbidity, accumulation of dampness and heat and phlegm and blood stasis were significantly lower than those of liver depression and spleen deficiency syndrome, while Simpson index was significantly higher(P<0.05). Compared with the accumulation of dampness and heat, the Ace and Chao1 indexes of the congestion of dampness turbidity and phlegm and blood stasis were significantly lower, and the Simpson index was significantly higher(P<0.05). The identification results of the characteristic gut microbiota of each TCM syndrome type showed that the abundance of Ruminococcus and Dorea genus in the gut microbiota of the congestion of dampness turbidity groupwas significantly increased. The abundance of Oscillospira and Akkermansia genus in the liver depression and spleen deficiency group was increased significantly. The abundance of Hemophilus and Agathobacter in the accumulation of dampness and heat group was increased significantly. The abundance of Alistipes genus in the phlegm and blood stasis group was significantly reduced, while the abundance of Streptococcus genus was significantly increased.Conclusion There are differences in diversity and structure ofgut microbiota among different TCM syndrome type, which may be involved in the occurrence and development of NASH and TCM syndromes.
-

-
表 1 各组患者一般资料的比较
组别 例数 男/女 年龄/岁 病程/年 湿浊内停证 21 12/9 32.0
(28.0~45.5)5.0
(2.5~9.0)肝郁脾虚证 16 5/11 32.5
(28.0~35.8)3.0
(2.0~4.8)湿热内蕴证 17 10/7 32.0
(32.0~40.5)5
(3.0~6.5)痰瘀互结证 20 11/9 39.0
(31.0~44.8)4.5
(3.0~6.8)表 2 各组患者肝功能水平的比较
U/L,X±S 组别 例数 AST ALT GGT ALP 湿浊内停证 21 132.52±31.51 159.90±17.372) 217.29±26.84 151.86±20.11 肝郁脾虚证 16 119.25±27.56 136.06±22.271) 206.00±34.40 149.75±23.41 湿热内蕴证 17 157.59±23.101)2) 162.24±28.521)2) 235.71±26.751)2) 150.06±29.39 痰瘀互结证 20 141.10±29.152) 158.15±34.551)2) 216.60±30.36 155.10±37.34 F 5.407 3.478 3.170 0.139 P 0.002 0.020 0.030 0.937 与湿浊内停证比较,1)P<0.05;与肝郁脾虚证比较,2)P<0.05。 表 3 各组患者血脂水平的比较
mmol/L,X±S 组别 例数 TG TC HDL-C LDL-C 湿浊内停证 21 3.56±1.461)2) 6.72±0.361) 1.83±0.24 3.84±0.51 肝郁脾虚证 16 2.31±0.33 6.21±0.68 1.90±0.23 3.85±0.33 湿热内蕴证 17 2.31±0.34 6.48±0.50 1.86±0.15 3.92±0.45 痰瘀互结证 20 3.28±1.511)2) 6.83±0.511)2) 1.78±0.26 4.06±0.59 F 6.141 5.098 2.355 0.819 P 0.001 0.003 0.079 0.488 与肝郁脾虚证比较,1)P<0.05;与湿热内蕴证比较,2)P<0.05。 表 4 各组患者肝纤维化指标的比较
ng/mL,X±S 组别 例数 透明质酸 层粘连蛋白 Ⅲ型前胶原蛋白 Ⅳ型胶原 湿浊内停证 21 97.85±13.832) 84.06±11.15 113.22±11.31 81.37±9.21 肝郁脾虚证 16 82.90±17.98 83.01±10.87 110.52±16.63 84.56±8.37 湿热内蕴证 17 93.20±10.24 85.10±10.41 116.35±15.86 81.45±9.84 痰瘀互结证 20 108.80±16.672) 108.38±31.121)2)3) 126.31±28.541)2) 100.39±28.421)2)3) F 9.268 8.239 5.432 5.783 P <0.001 <0.001 0.023 0.001 与湿浊内停证比较,1)P<0.05;与肝郁脾虚证比较,2)P<0.05;与湿热内蕴证比较,3)P<0.05。 表 5 各组患者CAP和LSM的比较
X±S 组别 例数 CAP/(dB/m) LSM/kPa 湿浊内停证 21 294.87±30.531) 5.44±1.051) 肝郁脾虚证 16 280.22±20.421) 5.32±0.991) 湿热内蕴证 17 289.44±23.381) 5.38±0.941) 痰瘀互结证 20 322.04±30.23 6.33±1.61 F 8.265 3.055 P <0.001 0.034 与痰瘀互结证比较,1)P<0.05。 -
[1] McPherson S, Armstrong MJ, Cobbold JF, et al. Quality standards for the management of non-alcoholic fatty liver disease(NAFLD): consensus recommendations from the British Association for the Study of the Liver and British Society of Gastroenterology NAFLD Special Interest Group[J]. Lancet Gastroenterol Hepatol, 2022, 7(8): 755-769. doi: 10.1016/S2468-1253(22)00061-9
[2] Tokushige K, Ikejima K, Ono M, et al. Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis 2020[J]. J Gastroenterol, 2021, 56(11): 951-963. doi: 10.1007/s00535-021-01796-x
[3] 刘云娜, 李帅广, 刘飞, 等. 肠道菌群代谢产物影响非酒精性脂肪肝的研究进展[J]. 食品与药品, 2022, 24(6): 583-588. https://www.cnki.com.cn/Article/CJFDTOTAL-SDPK202206013.htm
[4] 韦璐莹, 卢清华, 张扬武, 等. 基于"肠-肝轴"理论对非酒精性脂肪性肝病影响的研究进展[J]. 大众科技, 2022, 24(5): 88-91, 78. https://www.cnki.com.cn/Article/CJFDTOTAL-DZJI202205022.htm
[5] 顾立梅, 曹培让, 顾超, 等. 非酒精性脂肪肝中医证型及临床生化指标相关性研究[J]. 南京中医药大学学报, 2019, 35(6): 738-740. https://www.cnki.com.cn/Article/CJFDTOTAL-NJZY201906024.htm
[6] 袁维, 王炳予, 杨磊, 等. 芪参汤治疗非酒精性脂肪性肝炎的临床疗效观察及对肠道菌群的影响[J]. 中国中西医结合消化杂志, 2021, 29(6): 383-391. doi: 10.3969/j.issn.1671-038X.2021.06.02 https://zxyxh.whuhzzs.com/article/doi/10.3969/j.issn.1671-038X.2021.06.02
[7] 中华医学会肝病学分会脂肪肝和酒精性肝病学组, 中国医师协会脂肪性肝病专家委员会. 非酒精性脂肪性肝病防治指南(2018年更新版)[J]. 临床肝胆病杂志, 2018, 34(5): 947-957. https://www.cnki.com.cn/Article/CJFDTOTAL-CRBX201805002.htm
[8] 赵文霞, 许二平, 王宪波, 等. 非酒精性脂肪性肝炎中医诊疗指南[J]. 中西医结合肝病杂志, 2022, 32(11): 1059-1062. https://www.cnki.com.cn/Article/CJFDTOTAL-ZXGB202211028.htm
[9] 张声生, 李军祥. 非酒精性脂肪性肝病中医诊疗专家共识意见(2017)[J]. 中医杂志, 2017, 58(19): 1706-1710. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZYZ201719022.htm
[10] 魏倩, 郭津生. 非酒精性脂肪性肝病肝纤维化的发生机制、诊断与治疗[J]. 西南医科大学学报, 2020, 43(2): 97-102. https://www.cnki.com.cn/Article/CJFDTOTAL-LXYB202002002.htm
[11] 刘印聪, 罗金波, 张玉亭, 等. 肠道菌群代谢产物在非酒精性脂肪性肝病发病中的作用机制研究进展[J]. 山东医药, 2023, 63(5): 103-106. https://www.cnki.com.cn/Article/CJFDTOTAL-SDYY202305025.htm
[12] 钱林惠, 陈新利, 吴晖. 肠道菌群及其影响因素在非酒精性脂肪性肝病中的研究进展[J]. 国际消化病杂志, 2022, 42(6): 348-352. https://www.cnki.com.cn/Article/CJFDTOTAL-GWXH202206004.htm
[13] 王宇威, 刘近春, 安秀琴, 等. 肠道微生态与非酒精性脂肪性肝病研究进展[J]. 中国现代医生, 2022, 60(15): 192-196. https://www.cnki.com.cn/Article/CJFDTOTAL-ZDYS202215051.htm
[14] 朱彧, 何学敏, 陈明, 等. 降脂方对非酒精性脂肪肝的治疗效果及其对患者肠道菌群和代谢的影响[J]. 中国现代应用药学, 2022, 39(17): 2250-2256. https://www.cnki.com.cn/Article/CJFDTOTAL-XDYD202217012.htm
[15] 王炳予, 张雅丽, 杨磊, 等. 基于16S rRNA技术探讨芪参汤治疗非酒精性脂肪性肝纤维化的作用机制[J]. 海南医学院学报, 2020, 26(1): 18-24, 29. https://www.cnki.com.cn/Article/CJFDTOTAL-HNYY202001005.htm
[16] Vallianou N, Christodoulatos GS, Karampela I, et al. Understanding the Role of the Gut Microbiome and Microbial Metabolites in Non-Alcoholic Fatty Liver Disease: Current Evidence and Perspectives[J]. Biomolecules, 2021, 12(1): 56.
[17] 郭晓霞, 叶永安, 李小科, 等. 肝硬化患者中医证型演变过程中肠道菌群结构变化及其临床意义[J]. 中西医结合肝病杂志, 2022, 32(12): 1066-1072. https://www.cnki.com.cn/Article/CJFDTOTAL-ZXGB202212004.htm
[18] 吴巧玲. 非酒精性脂肪性肝病中医辨证分型与肠道菌群相关性的研究[D]. 南京: 南京中医药大学, 2022.
[19] Henke MT, Brown EM, Cassilly CD, et al. Capsular polysaccharide correlates with immune response to the human gut microbe Ruminococcus gnavus[J]. Proc Natl Acad Sci U S A, 2021, 118(20): e2007595118.
[20] Pal D, Naskar M, Bera A, et al. Chemical synthesis of the pentasaccharide repeating unit of the O-specific polysaccharide from Ruminococcus gnavus[J]. Carbohydr Res, 2021, 507: 108384.
[21] Parker BJ, Wearsch PA, Veloo A, et al. The Genus Alistipes: Gut Bacteria With Emerging Implications to Inflammation, Cancer, and Mental Health[J]. Front Immunol, 2020, 11: 906.
-




 下载:
下载: