Efficacy, safety and long-term prognosis of combined abiotic artificial liver in the treatment of chronic severe hepatitis
-
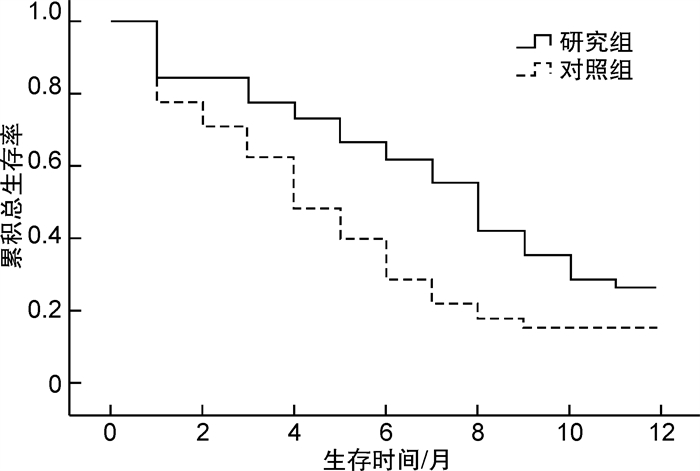
摘要: 目的 探讨组合型非生物型人工肝治疗慢性重型肝炎的有效性、安全性以及对患者长期预后的影响。方法 将纳入研究的所有慢性重型肝炎患者按随机数字表法分为研究组和对照组,对照组在内科综合治疗基础上加用单纯血浆置换治疗,研究组在内科综合治疗基础上加用组合型非生物型人工肝治疗,比较2组患者一般临床资料、治疗前后肝功能变化、治疗后短期疗效以及治疗后不良反应,采用Kaplan-Meier生存分析比较2组患者随访1年总生存率。结果 研究共前瞻性纳入慢性重型肝炎患者90例,其中男69例(76.7%),女21例(23.3%);年龄30~75岁,平均年龄(47.2±11.0)岁,中位年龄49岁;平均体重指数(22.5±3.1) kg/m2。对照组和研究组各45例,2组患者治疗后谷丙转氨酶、谷草转氨酶、总胆红素以及凝血酶原活动度较治疗前都有明显改善(P< 0.05),并且研究组患者治疗后上述指标的改善程度明显优于对照组(P< 0.05);治疗后研究组患者肝性脑病意识转清有效率为72.2%(26/36),肝肾综合征肾功能恢复有效率为31.8%(7/22),电解质紊乱纠正率为84.2%(32/38),腹水消退有效率为62.5%(25/40),明显高于对照组患者相对应的57.1%(20/35),9.5%(2/21),62.5%(25/40),47.4%(18/38)(均P< 0.05);Kaplan-Meier生存分析显示,研究组患者随访3、6、12个月的总生存率分别为82.3%、62.5%、28.6%,明显高于对照组患者的70.1%、38.9%、17.3%(χ2=5.913,P=0.015)。结论 组合型非生物型人工肝可有效改善慢性重型肝炎患者肝肾功能,明显提高患者远期生存率。
-
关键词:
- 组合型非生物型人工肝 /
- 慢性重型肝炎 /
- 长期预后
Abstract: Objective To investigate the efficacy, safety and long-term prognosis of combined abiotic artificial liver in the treatment of chronic severe hepatitis.Methods All patients with chronic severe hepatitis included in the study were divided into the study group and the control group by the random number table method. Both groups were complicated with different degrees of complications. The control group was treated with simple plasma exchange on the basis of comprehensive medical treatment, and the study group was treated with combined abiotic artificial liver on the basis of comprehensive medical treatment. The general clinical data, changes of liver function before and after treatment, short-term efficacy and adverse reactions after treatment were compared between the two groups. Kaplan-Meier survival analysis was used to compare the 1-year overall survival rate of patients between the two groups.Results A total of 90 patients with chronic severe hepatitis were prospectively included in the study, including 69 males(76.7%) and 21 females(23.3%), aged from 30 to 75 years, with an average age of (47.2 ± 11.0) years, a median age of 49 years and an average body mass index of (22.5±3.1) kg/m2. All patients were randomly divided into 45 cases(50%) in the control group and 45 cases(50%) in the study group. Alanine aminotransferase, aspartate aminotransferase, total bilirubin and prothrombin activity of the patients in the two groups after treatment, were significantly improved compared with those before treatment(P< 0.05), and all the above improvements in the study group were significantly better than those in the control group(P< 0.05). The consciousness conversion rate of hepatic encephalopathy in the study group was 72.2%(26/36), and the recovery rate of renal function in hepatorenal syndrome was 31.8%(7/22), the correction rate of electrolyte disorder was 84.2%(32/38), and the ascites regression rate was 62.5%(25/40), which was significantly higher than that of 57.1%(20/35), 9.5%(2/21), 62.5%(25/40), 47.4%(18/38) in the control group(P< 0.05) respectively. Kaplan-Meier survival analysis showed that the overall survival rate of patients in the study group on 3, 6, and 12 months' follow-up(82.3%, 62.5%, 28.6%) was significantly higher than that in the control group(70.1%, 38.9%, 17.3%)(χ2=5.913,P=0.015) respectively.Conclusion Combined abiotic artificial liver can effectively improve liver and kidney function and long-term survival rate of patients with chronic severe hepatitis. -

-
表 1 2组患者一般临床资料比较
例 基线资料 对照组
(n=45)研究组
(n=45)t/χ2 P 基线资料 对照组
(n=45)研究组
(n=45)t/χ2 P 性别 0.765 0.452 肝性脑病 0.772 0.449 男 34 35 是 35 36 女 11 10 否 10 9 年龄/岁 46.7±11.2 47.8±10.8 0.745 0.461 肝肾综合征 0.845 0.396 肝硬化病因 0.976 0.278 是 21 22 乙肝 27 28 否 24 23 丙肝 10 7 电解质紊乱 0.968 0.285 其他 8 10 是 40 38 食管胃底静脉 0.879 0.356 否 5 7 曲张程度 腹水 0.875 0.356 Ⅱ度 20 18 是 38 40 Ⅲ度 25 27 否 7 5 表 2 2组患者治疗前后肝功能比较
X±S 组别 谷丙转氨酶/(U·L-1) 谷草转氨酶/(U·L-1) 白蛋白/(g·L-1) 总胆红素/(μmol·L-1) 凝血酶原活动度/% 对照组 治疗前 146.4±34.2 164.3±38.4 22.3±4.7 146.5±45.7 37.8±5.7 治疗后 88.6±20.81) 96.2±18.91) 26.7±3.2 67.4±21.71) 46.9±6.61) 研究组 治疗前 151.6±35.7 172.8±42.3 22.5±4.9 157.8±46.2 36.9±6.2 治疗后 56.7±10.61)2) 61.5±12.31)2) 26.8±4.2 51.2±18.51)2) 53.5±6.71)2) 与本组治疗前比较,1)P < 0.05;与对照组治疗后比较,2)P < 0.05。 表 3 2组患者治疗后短期疗效比较
例 项目 对照组
(n=45)研究组
(n=45)χ2 P 肝性脑病意识转清 4.155 0.043 是 20 26 否 15 10 肝肾综合征肾功能恢复 3.876 0.048 是 2 7 否 19 15 电解质紊乱纠正 4.568 0.040 是 25 32 否 15 6 腹水消退 4.795 0.038 是 18 25 否 20 15 住院期间存活 2.344 0.097 是 35 38 否 10 7 表 4 2组患者治疗后不良反应比较
例 项目 对照组
(n=45)研究组
(n=45)χ2 P 皮疹 0.789 0.456 是 0 2 否 45 43 寒战 0.789 0.456 是 0 2 否 45 43 低血压 0.712 0.512 是 0 1 否 45 44 -
[1] 李志红. 慢性重症肝炎及失代偿期肝硬化患者医院内感染的现状原因及防治[J]. 中国医药指南, 2017, 15(12): 192. https://www.cnki.com.cn/Article/CJFDTOTAL-YYXK201712148.htm
[2] 李爽, 陈煜. 血浆紧缺情况下非生物型人工肝治疗新模式的探讨[J]. 临床肝胆病杂志, 2017, 33(9): 1687-1692. https://www.cnki.com.cn/Article/CJFDTOTAL-LCGD201709012.htm
[3] 杜卫星, 叶青, 李金科, 等. 血浆置换联合血浆吸附治疗慢性肝炎黄疸的临床观察[J]. 中国中西医结合消化杂志, 2018, 26(1): 40-42. http://zxpw.cbpt.cnki.net/WKD2/WebPublication/paperDigest.aspx?paperID=6e4bb97e-9f2c-43e1-8ecc-e45974dff401
[4] Tandon R, Froghi S. Artificial liver support systems[J]. J Gastroenterol Hepatol, 2021, 36(5): 1164-1179. doi: 10.1111/jgh.15255
[5] 兰玲鲜, 苏春雄. 非生物型人工肝对肝衰竭患者临床效果及预后的影响[J]. 河北医药, 2019, 41(4): 601-603. https://www.cnki.com.cn/Article/CJFDTOTAL-HBYZ201904032.htm
[6] 中华医学会感染病学分会肝衰竭与人工肝学组. 非生物型人工肝治疗肝衰竭指南(2016年版)[J]. 中华临床感染病杂志, 2016, 9(2): 97-103.
[7] Wu G, Wu D, Lo J, et al. A bioartificial liver support system integrated with a DLM/GelMA-based bioengineered whole liver for prevention of hepatic encephalopathy via enhanced ammonia reduction[J]. Biomater Sci, 2020, 8(10): 2814-2824. doi: 10.1039/C9BM01879D
[8] 杨文龙, 孙水林, 周锡进, 等. 终末期肝病模型评分与Child-Turcotte-Pugh分级对非生物型人工肝治疗乙型肝炎相关性肝衰竭患者预测价值的研究[J]. 中华危重症医学杂志(电子版), 2016, 9(1): 20-27. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWZD201601006.htm
[9] Shang J, Wang M, Wen Q, et al. A novel prognostic model to predict outcome of artificial liver support system treatment[J]. Sci Rep, 2021, 11(1): 7510. doi: 10.1038/s41598-021-87055-8
[10] Bertani H, Gelmini R, Del Buono MG, et al. Literature overview on artificial liver support in fulminant hepatic failure: a methodological approach[J]. Int J Artif Organs, 2002, 25(10): 903-910. doi: 10.1177/039139880202501002
[11] 徐燕梅, 黄国峰. 人工肝治疗机双重血浆置换治疗PBC皮肤瘙痒症的护理[J]. 黑龙江科学, 2019, 10(4): 80-81. https://www.cnki.com.cn/Article/CJFDTOTAL-HELJ201904038.htm
[12] Zhang HF, Xie ZY, Ouyang XX, et al. Accuracy of pipeline blood glucose monitoring in patients with severe liver injury undergoing artificial liver support system treatment[J]. Hepatobiliary Pancreat Dis Int, 2019, 18(5): 484-487. doi: 10.1016/j.hbpd.2019.08.002
[13] 危敏, 彭虹, 熊庭婷, 等. 新型人工肝组合技术双重血浆分子吸附联合血浆置换与单纯血浆置换治疗肝衰竭[J]. 中国组织工程研究, 2019, 23(14): 2235-2240. https://www.cnki.com.cn/Article/CJFDTOTAL-XDKF201914018.htm
[14] Yang CF, Zhang Z, Zhang XY, et al. Artificial liver support system in pediatric acute liver failure due to mushroom poisoning: Case series[J]. Ann Hepatol, 2021, 23: 100290. doi: 10.1016/j.aohep.2020.100290
[15] Ma Y, Chen F, Liu C, et al. A novel predictive score for citrate accumulation among patients receiving artificial liver support system therapy with regional citrate anticoagulation[J]. Sci Rep, 2020, 10(1): 12861. doi: 10.1038/s41598-020-69902-2
-




 下载:
下载: