-
摘要: 目的 探讨结直肠管状绒毛状腺瘤发生的相关危险因素。方法 将2022年4月—2023年4月于江苏省中医院消化内镜中心住院接受结肠镜下息肉治疗,并经内镜下手术所取标本病理确诊的228例患者纳为研究对象,其中管状腺瘤患者131例,管状绒毛状腺瘤患者97例,通过单因素分析比较两组间年龄、性别、吸烟史、饮酒史、肠癌家族史、BMI、高血压、糖尿病、高脂血症、病变部位、天冬氨酸氨基转移酶、丙氨酸氨基转移酶、尿素、肌酐、总胆固醇、甘油三酯、高密度脂蛋白胆固醇、低密度脂蛋白胆固醇、糖化血红蛋白方面的差异,并通过二分类logistic回归分析明确结直肠管状绒毛状腺瘤发生的危险因素。结果 在单因素分析中,两组的年龄、性别、吸烟史、饮酒史、BMI、高血压、糖尿病、高脂血症、血清学指标比较均差异无统计学意义(均P>0.05);两组在是否有肠癌家族史、病变部位是否在肝曲、横结肠和降结肠比较中差异有统计学意义(P<0.05);年龄作为危险因素差异有统计学意义,通过二分类logistic分析显示,肠癌家族史(OR=7.838,95%CI:2.205~27.859,P=0.001)、年龄(OR=1.032,95%CI:1.003~1.062,P=0.031)、病变部位在横结肠(OR=0.277,95%CI:0.092~0.836,P=0.023)与结直肠管状绒毛状腺瘤的发生有关。结论 患者的年龄、有无肠癌家族史和病变部位为横结肠是结直肠管状绒毛状腺瘤发生的相关危险因素,应对病理类型为结直肠管状绒毛状腺瘤患者的降结肠、肝曲在行肠镜检查过程中加强关注。Abstract: Objective To explore the relevant risk factors for the occurrence of colonic villous adenoma.Methods Two hundred and twenty-eight patients who underwent colonoscopic polyp treatment at the Digestive Endoscopy Center of Jiangsu Provincial Hospital of Traditional Chinese Medicine from April 2022 to April 2023 and were pathologically confirmed through endoscopic surgery were included in this study. Among them, 131 patients with tubular adenoma and 97 patients with tubular villous adenoma were compared between the two groups in terms of age, gender, smoking history, drinking history, family history of bowel cancer, BMI, hypertension, diabetes, hyperlipidemia, lesion site, aspartate aminotransferase, alanine aminotransferase, urea, creatinine, total cholesterol, triglyceride, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol Differences in glycosylated hemoglobin were identified through binary logistic regression analysis to identify risk factors for the development of colorectal villous adenoma.Results In the univariate analysis, there was no significant difference between the two groups in age, sex, smoking history, drinking history, BMI, hypertension, diabetes, hyperlipidemia, and serological indicators(P>0.05); there was a statistically significant difference(P<0.05) between the two groups in whether they had a family history of colon cancer and whether the lesion was located in the liver curvature, transverse colon, and descending colon; there is a statistically significant difference in age as a risk factor. Through binary logistic analysis, it was found that a family history of colorectal cancer(OR=7.838, 95%CI: 2.205-27.859, P=0.001), age(OR=1.032, 95%CI: 1.003-1.062, P=0.031), and lesion location in the transverse colon(OR=0.277, 95%CI: 0.092-0.836, P=0.023) are associated with the occurrence of colorectal tubular villous adenoma.Conclusion The age of the patient, family history of colorectal cancer, and the location of the lesion in the transverse colon are related risk factors for the occurrence of colorectal tubular villous adenoma; Moreover, it is necessary to strengthen attention during the colonoscopy examination of patients with colorectal villous adenoma and liver curvature.
-
Key words:
- colorectal polyps /
- tubular adenoma /
- tubular villous adenoma /
- metabolic syndrome /
- risk factors
-

-
表 1 两组患者的年龄分布情况
例(%) 年龄/岁 管状腺瘤组
(n=131)管状绒毛状腺瘤组
(n=97)合计 21~30 2(0.88) 1(0.44) 3(1.32) >30~40 6(2.63) 4(1.75) 10(4.39) >40~50 17(7.46) 8(3.51) 25(10.96) >50~60 52(22.81) 34(14.91) 86(37.72) >60~70 44(19.30) 34(14.91) 78(34.21) >70 10(4.39) 16(7.02) 26(11.40) 表 2 不同类型结直肠腺瘤患者的危险因素单因素分析
X±S,例(%),M(P25,P75) 危险因素 管状腺瘤组(n=131) 管状绒毛状腺瘤组(n=97) t/χ2 P 年龄/岁 57.73±10.25 60.77±10.98 -2.210 0.394 性别 男 85(64.89) 60(61.86) 0.221 0.638 女 46(35.11) 37(38.14) 高血压 0.185 0.667 有 49(37.40) 39(40.21) 无 82(62.60) 58(59.79) 糖尿病 0.041 0.840 有 16(12.21) 11(11.34) 无 115(87.79) 86(88.66) 高脂血症 0.074 0.785 有 15(11.45) 10(10.31) 无 116(88.55) 87(89.69) 吸烟史 -0.001 0.999 有 27(20.61) 20(20.62) 无 104(79.39) 77(79.38) 饮酒史 -0.855 0.392 有 20(15.27) 19(19.59) 无 111(84.73) 78(80.41) 肠癌家族史 8.233 0.004 有 5(3.82) 14(14.43) 无 126(96.18) 83(85.57) BMI 25.57±3.16 24.23±3.02 0.632 0.616 AST/(U/L) 19.00(14.00,26.00) 19.00(15.00,24.00) -0.102 0.919 ALT/(U/L) 19.00(15.00,24.00) 17.00(12.50,24.50) -1.695 0.090 Ure/(mmol/L) 5.11(4.37,6.25) 5.30(4.48,6.12) -0.339 0.734 Cr/(μmmol/L) 69.35(61.00,80.02) 67.40(60.00,81.85) -0.308 0.758 TC/(mmol/L) 4.50±8.99 4.65±1.02 -0.577 0.595 TG/(mmol/L) 1.50(1.01,2.10) 1.29(0.93,1.99) -1.453 0.146 HDL-C/(mmol/L) 1.19(1.01,1.42) 1.27(1.05,1.47) -1.765 0.078 LDL-C/(mmol/L) 2.57±0.77 2.68±0.81 -0.819 0.211 HbA1c/% 5.80(5.50,6.10) 5.70(5.40,6.00) -0.707 0.480 表 3 不同类型结直肠腺瘤病变部位分析
处(%) 病变部位 管状腺瘤组(234处) 管状绒毛状腺瘤组(105处) Z P 肝曲 26(11.11) 2(1.90) -4.037 < 0.01 横结肠 46(19.66) 8(7.62) -4.707 < 0.01 回盲部 14(5.98) 6(5.71) -1.185 0.236 降结肠 27(11.54) 3(2.86) -3.860 < 0.01 降乙交界 0 1(0.95) -1.162 0.245 盲肠 1(0.43) 1(0.95) -0.214 0.831 脾曲 2(0.85) 3(2.86) -0.797 0.426 升结肠 32(13.68) 16(15.24) -1.449 0.147 乙状结肠 63(26.92) 36(34.29) -1.650 0.099 直肠 20(8.55) 23(21.90) -1.608 0.108 直乙交界 3(1.28) 6(5.71) -1.490 0.136 表 4 危险因素二分类logistic回归分析
影响因素 β SE Wald χ2 P OR 95%CI 年龄 0.032 0.015 4.627 0.031 1.032 1.003~1.062 肠癌家族史 2.059 0.647 10.128 0.001 7.838 2.205~27.859 病变部位在肝曲 -2.787 1.626 2.936 0.087 0.062 0.003~1.493 病变部位在横结肠 -1.283 0.563 5.189 0.023 0.277 0.092~0.836 病变部位在降结肠 1.132 1.526 0.550 0.458 3.102 0.156~61.743 常量 -1.975 0.898 4.840 0.028 0.139 -
[1] Lee SY, Song WH, Oh SC, et al. Anatomical distribution and detection rate of colorectal neoplasms according to age in the colonoscopic screening of a Korean population[J]. Ann Surg Treat Res, 2018, 94(1): 36-43. doi: 10.4174/astr.2018.94.1.36
[2] 中国中西医结合学会消化内镜学专业委员会大肠早癌专家委员会, 张北平, 魏玮, 等. 结直肠腺瘤及早期结直肠癌中西医结合诊治专家共识(2021)[J]. 中医杂志, 2022, 63(10): 989-997. doi: 10.13288/j.11-2166/r.2022.10.017
[3] 徐舒佳, 李燕飞, 刘晓明, 等. 早期结肠癌经肠镜检查的准确度情况及作用价值分析[J]. 中国中西医结合消化杂志, 2019, 27(7): 530-533. https://zxyxh.whuhzzs.com/article/doi/10.3969/j.issn.1671-038X.2019.07.11
[4] 中华医学会消化内镜学分会结直肠学组, 刘思德, 令狐恩强, 等. 结肠镜检查肠道准备专家共识意见(2023, 广州)[J]. 中华消化内镜杂志, 2023, 40(6): 421-430. doi: 10.3760/cma.j.cn321463-20230607-00230
[5] 刘宗超, 李哲轩, 张阳, 等. 2020全球癌症统计报告解读[J]. 肿瘤综合治疗电子杂志, 2021, 7(2): 1-14. https://www.cnki.com.cn/Article/CJFDTOTAL-ZLZD202102001.htm
[6] Siegel RL, Miller KD, Goding Sauer A, et al. Colorectal cancer statistics, 2020[J]. CA Cancer J Clin, 2020, 70(3): 145-164. doi: 10.3322/caac.21601
[7] 朱雄增. 胃肠道癌前病变和癌的WHO诊断新标准[J]. 中华病理学杂志, 2003, 32(2): 168-169. doi: 10.3760/j.issn:0529-5807.2003.02.020
[8] 孔娜, 缪应雷, 何利平, 等. 大肠息肉癌变的影响因素[J]. 昆明医科大学学报, 2023, 44(4): 53-61. https://www.cnki.com.cn/Article/CJFDTOTAL-KMYX202304008.htm
[9] 田晓彤, 卜淑蕊. 结直肠息肉的临床特征研究[J]. 临床内科杂志, 2022, 39(2): 91-94. https://www.cnki.com.cn/Article/CJFDTOTAL-LCLZ202202006.htm
[10] Morita T, Tabata S, Mineshita M, et al. The metabolic syndrome is associated with increased risk of colorectal adenoma development: the Self-Defense Forces health study[J]. Asian Pac J Cancer Prev, 2005, 6(4): 485-489.
[11] 虞晨燕, 朱锦舟, 刘晓琳, 等. 结直肠腺瘤相关危险因素分析及预测模型构建[J]. 中国中西医结合消化杂志, 2021, 29(7): 507-511. doi: 10.3969/j.issn.1671-038X.2021.07.13
[12] 刘志威, 赵利婷, 余志荣, 等. 代谢综合征对结直肠管状绒毛状腺瘤的影响因素分析[J]. 中华消化病与影像杂志(电子版), 2022, 12(4): 215-219. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHYE202204005.htm
[13] 吴娟. 代谢综合征组分与结直肠腺瘤性息肉的关系[J]. 中国慢性病预防与控制, 2013, 21(3): 359-360. https://www.cnki.com.cn/Article/CJFDTOTAL-ZMXB201303047.htm
[14] Milano A, Bianco MA, Buri L, et al. Metabolic syndrome is a risk factor for colorectal adenoma and cancer: a study in a White population using the harmonized criteria[J]. Therap Adv Gastroenterol, 2019, 12: 1756284819867839.
[15] 方崇文, 张焰平, 孙小明, 等. 腺瘤型肠息肉发生的影响因素分析[J]. 中国医药导报, 2022, 19(13): 104-106. https://www.cnki.com.cn/Article/CJFDTOTAL-YYCY202213021.htm
[16] 李雪, 陈春华. 代谢综合征组分与结直肠腺瘤临床病理特征的相关性[J]. 胃肠病学, 2019, 24(6): 350-354. https://www.cnki.com.cn/Article/CJFDTOTAL-WIEC201906009.htm
[17] 董晓宇, 徐世平, 石卉, 等. 结直肠良恶性息肉患者脂代谢特征分析[J]. 解放军医学院学报, 2023, 44(6): 575-580, 593. https://www.cnki.com.cn/Article/CJFDTOTAL-JYJX202306001.htm
[18] 雷甜甜, 刘家欢, 黄虹玉, 等. 进展期结直肠腺瘤及高危腺瘤的危险因素分析[J]. 中华胃肠内镜电子杂志, 2021, 8(2): 61-67. https://www.cnki.com.cn/Article/CJFDTOTAL-WCNJ202102004.htm
[19] Song MY, Emilsson L, Roelstraete B, et al. Risk of colorectal cancer in first degree relatives of patients with colorectal polyps: nationwide case-control study in Sweden[J]. BMJ, 2021, 373: n877.
[20] 张燕萍, 李西梅. 两个年龄组结肠息肉的临床特征分析[J]. 宁夏医学杂志, 2011, 33(1): 56-57. https://www.cnki.com.cn/Article/CJFDTOTAL-NXYX201101034.htm
[21] 胡娜, 叶长根, 冷芳. 结肠息肉的病理特点与年龄、性别关系研究分析[J]. 江西医药, 2021, 56(12): 2216-2218. https://www.cnki.com.cn/Article/CJFDTOTAL-JXYY202112035.htm
[22] 张舒琪, 李国熊, 叶孝乾. 结直肠上皮内瘤变分级的临床病理特点分析[J]. 中国中西医结合消化杂志, 2021, 29(9): 646-650. 10.3969/j.issn.1671-038X.2021.09.10
[23] 兰琴, 魏玉霞. 影响结肠腺瘤发病的危险因素及预防术后复发研究进展[J]. 中国中西医结合消化杂志, 2021, 29(8): 595-598. https://zxyxh.whuhzzs.com/article/doi/10.3969/j.issn.1671-038X.2021.08.14
[24] 范宝峰, 李真真, 王洁, 等. 553例经结肠镜检出肿瘤性息肉的患者年龄与性别分布特征分析[J]. 当代医学, 2022, 28(21): 60-62. https://www.cnki.com.cn/Article/CJFDTOTAL-DDYI202221017.htm
[25] 黄晗, 刘美, 慈新宇, 等. 结直肠息肉癌变相关因素的分析[J]. 山东第一医科大学(山东省医学科学院)学报, 2023, 44(2): 142-146. https://www.cnki.com.cn/Article/CJFDTOTAL-TSYX202302010.htm
[26] 杨伟, 陈洁静. 雌激素受体β与结直肠癌临床病理特征及预后关系的Meta分析[J]. 中华普通外科学文献(电子版), 2020, 14(6): 475-480. https://www.cnki.com.cn/Article/CJFDTOTAL-ZHPD202006022.htm
[27] 庄云英, 张海燕, 曾清芳. 雌激素及其受体在胃肠道疾病中的作用[J]. 现代消化及介入诊疗, 2020, 25(6): 816-818. https://www.cnki.com.cn/Article/CJFDTOTAL-XDXH202006031.htm
-

| 引用本文: | 李慧, 肖君, 郭欣, 等. 结直肠管状绒毛状腺瘤发生的相关危险因素分析[J]. 中国中西医结合消化杂志, 2023, 31(11): 879-883. doi: 10.3969/j.issn.1671-038X.2023.11.11 |
| Citation: | LI Hui, XIAO Jun, GUO Xin, et al. Analysis of relevant risk factors for the occurrence of colonic villous adenoma[J]. Chin J Integr Tradit West Med Dig, 2023, 31(11): 879-883. doi: 10.3969/j.issn.1671-038X.2023.11.11 |
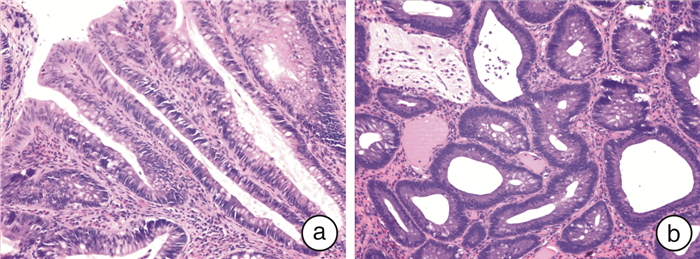
- Figure 1.



 下载:
下载: