Fecal microbiota transplantation for constipation in patients with parkinson disease: clinical efficacy observation
-
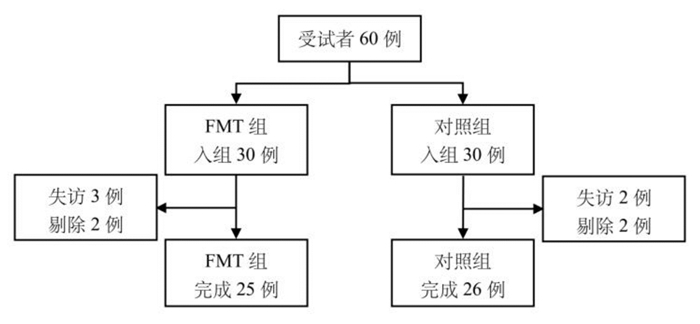
摘要: 目的 探讨肠道菌群移植(fecal microbiota transplantation,FMT)对便秘合并帕金森病(parkinson disease,PD)患者肠道便秘症状及左旋多巴疗效的影响,为临床治疗提供参考。方法 纳入2020年10月—2021年12月招募诊断的51例PD患者为研究对象,随机分为FMT组(n=25)与对照组(n=26),两组均予左旋多巴常规治疗,FMT组在此基础上加用粪菌胶囊调整肠道菌群,对照组给予空白胶囊,采用便秘患者生活质量量表(patient-assessment of constipation quality of life,PAC-QOL)等评估患者便秘症状及满意度,采用统一PD评定量表(UPDRS-Ⅲ)等评估两组患者治疗前后的运动症状及心理状态。结果 ① 与治疗前及对照组比较,FMT组的PAC-QOL、Bristol粪便性状量表评分改善显著,差异有统计学意义(P<0.05);②与治疗前比较,两组患者的UPDRS-Ⅲ评分均有改善,FMT组差异有统计学意义(P<0.05);③与对照组比较,治疗后FMT组的匹兹堡睡眠质量指数评分下降,差异有统计学意义(P<0.05)。结论 FMT干预能有效改善PD患者的便秘症状及睡眠质量,可能有增强左旋多巴对运动症状的疗效,但远期影响仍有待研究。Abstract: Objective This study aims to explore the impact of fecal microbiota transplantation(FMT) on gastrointestinal constipation symptoms and levodopa efficacy in patients afflicted by parkinson disease and constipation, to provideclinical insights for treatment.Methods A total of 51 diagnosed parkinson disease patients recruited from October 2020 to December 2021 in our hospital were randomly divided into the FMT group(n=25) and the control group(n=26). Both groups received routine treatment with levodopa. In the FMT group, fecal microbiota was adjusted by using fecal microbiota capsules in addition to levodopa treatment, while the control group was given blank capsule. Constipation symptoms and satisfaction were evaluated using the patient assessment of constipation quality of life(PAC-QOL) questionnaire, and motor symptoms and psychological status before and after treatment were assessed using the unified parkinson disease rating scale part Ⅲ(UPDRS-Ⅲ).Results In the FMT group, compared to before treatment and the control group, the PAC-QOL and bristol stool form scale(BSFS) scores improved significantly(P<0.05); both groups showed improvement in UPDRS-Ⅲ motor scores compared to before treatment, with a statistically significant difference in the FMT group(P<0.05); after treatment, the pittsburgh sleep quality index(PSQI) score decreased significantly in the FMT group compared to the control group(P<0.05).Conclusion FMT intervention can effectively improve constipation symptoms and sleep quality in parkinson disease patients. It may enhance the efficacy of levodopa on motor symptoms, but the long-term effects remain to be studied.
-
Key words:
- parkinson disease /
- constipation /
- fecal microbiota transplantation
-

-
表 1 两组PD患者的一般资料比较
例,X±S 一般资料 FMT组
(n=25)对照组
(n=26)P 性别 0.683 男 13 15 女 12 11 年龄/岁 70.88±10.92 73.77±13.19 0.399 病程/年 3.44±1.76 3.88±1.93 0.394 PAC-QOL/分 45.96±11.84 46.38±10.89 0.386 BSFS/分 1.56±0.65 1.58±0.76 0.932 UPDRS-Ⅲ/分 42.40±11.29 41.73±10.49 0.386 ADL/分 18.56±5.77 19.35±4.43 0.587 MMSE/分 25.68±2.87 25.14±3.00 0.526 MoCA/分 21.92±2.57 21.62±2.68 0.681 PSQI/分 9.24±2.77 10.38±3.79 0.225 每周排便次数/次 1.88±1.13 1.62±1.36 0.454 表 2 两组PD患者治疗前后排便情况比较
X±S 指标 FMT组(n=25) 对照组(n=26) 治疗前 治疗后 治疗前 治疗后 每周排便次数/次 1.88±1.13 3.40±1.161)2) 1.62±1.36 1.69±0.93 BSFS/分 1.56±0.65 2.88±0.881)2) 1.58±0.76 1.73±0.67 与本组治疗前比较,1)P<0.05;与对照组治疗后比较,2)P<0.05。 表 3 两组PD患者治疗前后PAC-QOL总评分比较
分,X±S 组别 例数 治疗前 治疗后 P FMT组 25 45.96±11.84 32.88±9.43 < 0.05 对照组 26 46.38±10.89 45.73±9.57 0.302 P 0.894 < 0.05 表 4 两组PD患者各项量表评分的比较
分,X±S 量表 FMT组(n=25) 对照组(n=26) 治疗前 治疗后 治疗前 治疗后 UPDRS-Ⅲ 42.40±11.29 39.40±9.691) 41.73±10.49 41.12±9.61 ADL 18.56±5.77 17.32±3.871) 19.35±4.43 18.23±4.38 MMSE 25.68±2.87 25.48±2.68 25.14±3.00 24.96±2.85 MoCA 21.92±2.57 21.60±2.35 21.62±2.68 21.54±2.35 PSQI 9.24±2.77 8.24±2.541)2) 10.38±3.79 10.08±3.03 与本组治疗前比较,1)P<0.05;与对照组治疗后比较,2)P<0.05。 -
[1] Barichella M, Cereda E, Pezzoli G. Major nutritional issues in the management of Parkinson's disease[J]. Mov Disord, 2009, 24(13): 1881-1892. doi: 10.1002/mds.22705
[2] Pfeiffer RF. Gastrointestinal dysfunction in parkinson's disease[J]. Curr Treat Options Neurol, 2018, 20(12): 54. doi: 10.1007/s11940-018-0539-9
[3] Berg D, Postuma RB, Adler CH, et al. MDS research criteria for prodromal Parkinson's disease[J]. Mov Disord, 2015, 30(12): 1600-1611. doi: 10.1002/mds.26431
[4] Keshavarzian A, Green SJ, Engen PA, et al. Colonic bacterial composition in Parkinson's disease[J]. Mov Disord, 2015, 30(10): 1351-1360. doi: 10.1002/mds.26307
[5] Forsyth CB, Shannon KM, Kordower JH, et al. Increased intestinal permeability correlates with sigmoid mucosa alpha-synuclein staining and endotoxin exposure markers in early Parkinson's disease[J]. PLoS One, 2011, 6(12): e28032. doi: 10.1371/journal.pone.0028032
[6] Shanahan F, Quigley EM. Manipulation of the microbiota for treatment of IBS and IBD-challenges and controversies[J]. Gastroenterology, 2014, 146(6): 1554-1563. doi: 10.1053/j.gastro.2014.01.050
[7] Sampson TR, Debelius JW, Thron T, et al. Gut microbiota regulate motor deficits and neuroinflammation in a model of parkinson's disease[J]. Cell, 2016, 167(6): 1469-1480. e12. doi: 10.1016/j.cell.2016.11.018
[8] Braak H, de Vos RA, Bohl J, et al. Gastric alpha-synuclein immunoreactive inclusions in Meissner's and Auerbach's plexuses in cases staged for Parkinson's disease-related brain pathology[J]. Neurosci Lett, 2006, 396(1): 67-72. doi: 10.1016/j.neulet.2005.11.012
[9] Hong CT, Chen JH, Huang TW. Probiotics treatment for Parkinson disease: a systematic review and meta-analysis of clinical trials[J]. Aging, 2022, 14(17): 7014-7025. doi: 10.18632/aging.204266
[10] Sun MF, Zhu YL, Zhou ZL, et al. Neuroprotective effects of fecal microbiota transplantation on MPTP-induced Parkinson's disease mice: gut microbiota, glial reaction and TLR4/TNF-α signaling pathway[J]. Brain Behav Immun, 2018, 70: 48-60. doi: 10.1016/j.bbi.2018.02.005
[11] Zhang TM, Yu SY, Guo P, et al. Nonmotor symptoms in patients with Parkinson disease: a cross-sectional observational study[J]. Medicine(Baltimore), 2016, 95(50): e5400.
[12] Challis C, Hori A, Sampson TR, et al. Gut-seeded α-synuclein fibrils promote gut dysfunction and brain pathology specifically in aged mice[J]. Nat Neurosci, 2020, 23(3): 327-336. doi: 10.1038/s41593-020-0589-7
[13] Abbott RD, Petrovitch H, White LR, et al. Frequency of bowel movements and the future risk of Parkinson's disease[J]. Neurology, 2001, 57(3): 456-462. doi: 10.1212/WNL.57.3.456
[14] Petrovitch H, Abbott RD, Ross GW, et al. Bowel movement frequency in late-life and substantia nigra neuron density at death[J]. Mov Disord, 2009, 24(3): 371-376. doi: 10.1002/mds.22360
[15] Barichella M, Severgnini M, Cilia R, et al. Unraveling gut microbiota in Parkinson's disease and atypical Parkinsonism[J]. Mov Disord, 2019, 34(3): 396-405. doi: 10.1002/mds.27581
[16] Yang XD, Ai PH, He XQ, et al. Parkinson's disease is associated with impaired gut-blood barrier for short-chain fatty acids[J]. Mov Disord, 2022, 37(8): 1634-1643. doi: 10.1002/mds.29063
[17] Fang X. Potential role of gut microbiota and tissue barriers in Parkinson's disease and amyotrophic lateral sclerosis[J]. Int J Neurosci, 2016, 126(9): 771-776. doi: 10.3109/00207454.2015.1096271
[18] Zhao Z, Ning JW, Bao XQ, et al. Fecal microbiota transplantation protects rotenone-induced Parkinson's disease mice via suppressing inflammation mediated by the lipopolysaccharide-TLR4 signaling pathway through the microbiota-gut-brain axis[J]. Microbiome, 2021, 9(1): 226. doi: 10.1186/s40168-021-01107-9
[19] Yang XD, Qian YW, Xu SQ, et al. Longitudinal analysis of fecal microbiome and pathologic processes in a rotenone induced mice model of parkinson's disease[J]. Front Aging Neurosci, 2017, 9: 441.
[20] Nielsen HH, Qiu J, Friis S, et al. Treatment for Helicobacter pylori infection and risk of Parkinson's disease in Denmark[J]. Eur J Neurol, 2012, 19(6): 864-869. doi: 10.1111/j.1468-1331.2011.03643.x
[21] Devos D, Lebouvier T, Lardeux B, et al. Colonic inflammation in Parkinson's disease[J]. Neurobiol Dis, 2013, 50: 42-48. doi: 10.1016/j.nbd.2012.09.007
[22] Fasano A, Bove F, Gabrielli M, et al. The role of small intestinal bacterial overgrowth in Parkinson's disease[J]. Mov Disord, 2013, 28(9): 1241-1249. doi: 10.1002/mds.25522
[23] Holmqvist S, Chutna O, Bousset L, et al. Direct evidence of Parkinson pathology spread from the gastrointestinal tract to the brain in rats[J]. Acta Neuropathol, 2014, 128(6): 805-820. doi: 10.1007/s00401-014-1343-6
[24] Ananthaswamy A. Faecal transplant eases symptoms of Parkinson's disease[J]. New Sci, 2011, 209(2796): 8-9. doi: 10.1016/S0262-4079(11)60124-3
[25] Maini Rekdal V, Bess EN, Bisanz JE, et al. Discovery and inhibition of an interspecies gut bacterial pathway for Levodopa metabolism[J]. Science, 2019, 364(6445): eaau6323. doi: 10.1126/science.aau6323
[26] Barichella M, Pacchetti C, Bolliri C, et al. Probiotics and prebiotic fiber for constipation associated with Parkinson disease: an RCT[J]. Neurology, 2016, 87(12): 1274-1280. doi: 10.1212/WNL.0000000000003127
-




 下载:
下载: