Effect of spleen deficiency syndrome on intestinal uric acid excretion in hyperuricemia mice
-
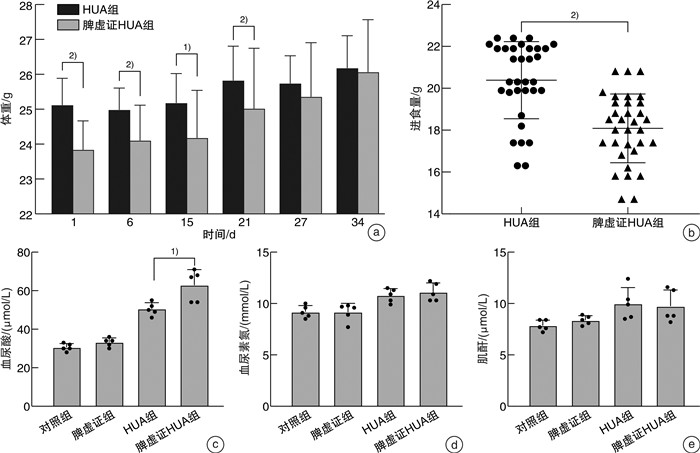
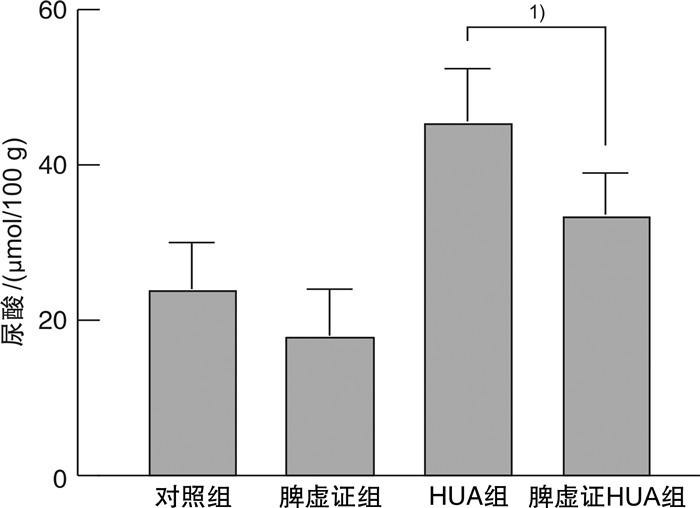
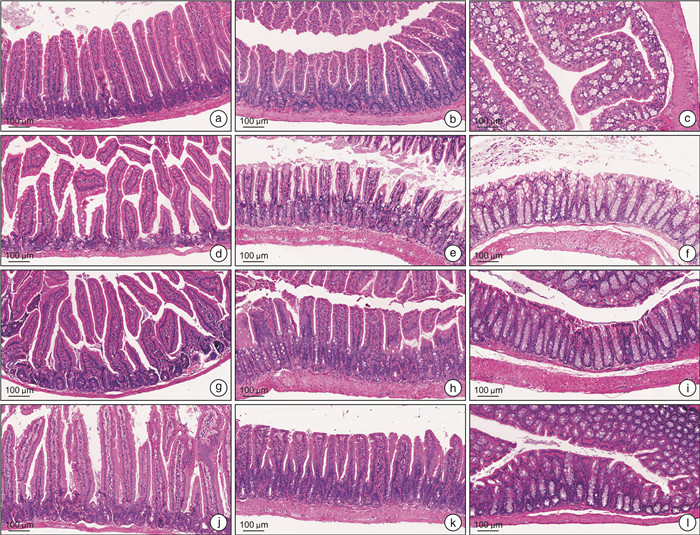
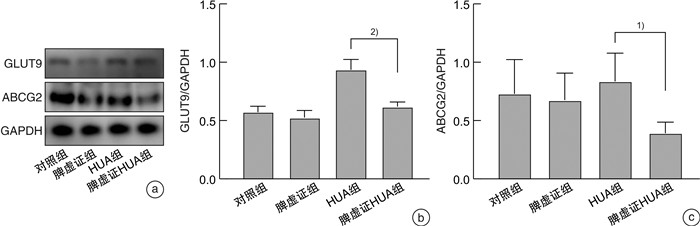
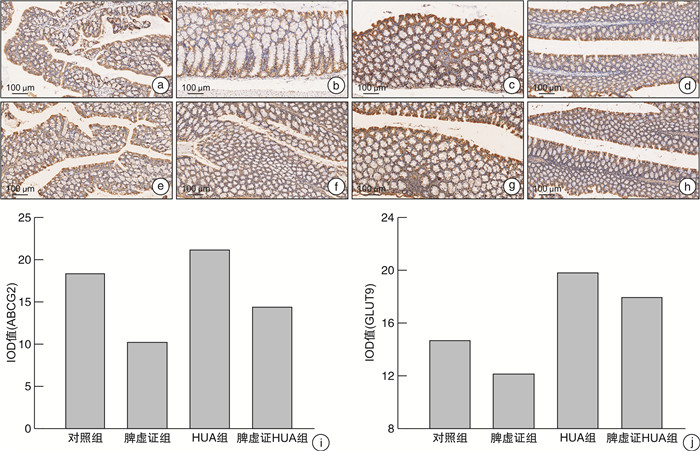
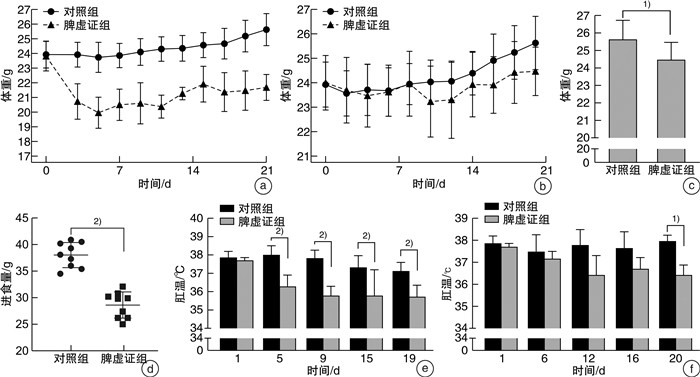
摘要: 目的 比较脾虚证高尿酸血症(hyperuricemia,HUA)小鼠及非脾虚证HUA小鼠的血尿酸水平、粪便尿酸水平、各段肠道形态学变化、肠道尿酸转运体ABCG2及GLUT9表达的改变,探讨脾虚证影响尿酸代谢的途径及机制。方法 将小鼠随机分为对照组、脾虚证组、HUA组及脾虚证HUA组,以多因素伤脾制作脾虚证模型,以2%尿酸+3%氧嗪酸钾饲料制作HUA模型。脾虚证造模过程中监测小鼠体重、进食量及肛温。造模结束后取血标本检测血尿酸、血尿素氮等指标,取粪便检测粪便尿酸水平,取空肠、回肠及结肠组织行苏木精-伊红染色,Western Blot及免疫组化检测结肠组织中ABCG2及GLUT9蛋白的表达。结果 脾虚证模型评估:与对照组小鼠比较,脾虚证组小鼠体重减轻(P < 0.05),进食量显著减少(P < 0.01),肛温下降(P < 0.05)。HUA造模期间,脾虚证HUA组小鼠体重逐渐上升,造模结束后体重与对照组比较差异无统计学意义。脾虚证HUA组小鼠血尿酸水平较HUA组升高(P < 0.05),尿素氮及肌酐水平4组比较差异无统计学意义。粪便尿酸水平:脾虚证HUA组小鼠粪便尿酸水平较HUA组明显降低(P < 0.05)。苏木精-伊红染色可见脾虚证组回肠及结肠组织绒毛缩短,排列松散;脾虚证HUA组空肠及回肠组织绒毛排列松散,结肠组织杯状细胞减少。Western Blot结果显示,与HUA组比较,脾虚证HUA组结肠组织中ABCG2及GLUT9的表达降低。免疫组化结果显示,与对照组比较,HUA组小鼠结肠组织中ABCG2及GLUT9的表达增多;与HUA组比较,脾虚证HUA组小鼠结肠中ABCG2及GLUT9的表达下降。结论 脾虚证HUA小鼠肠道尿酸排泄障碍导致血尿酸水平升高,可能与肠道尿酸转运蛋白ABCG2及GLUT9表达下降相关。Abstract: Objective To explore the mechanism of the effect of spleen deficiency syndrome on uric acid metabolism from the blood uric acid level, fecal uric acid level, intestinal morphological changes, and the expression of intestinal uric acid transporter ABCG2 and GLUT9.Methods Mice were randomly divided into blank group, spleen deficiency group, HUA group and spleen deficiency HUA group. The spleen deficiency syndrome model was made with compound spleen injury factors, and the HUA model was made with 2% uric acid +3% potassium oxazinate feed. Anal temperature, body weight and diet of mice were monitored during spleen deficiency modeling. Blood samples were collected to detect uric acid and urea nitrogen, stool was collected to detect fecal uric acid level. The tissues of jejunum, ileum and colon were stained with Hematoxylin Eosin staining(HE) and the protein expression of ABCG2 and GLUT9 were detected by Western Blot.Results Evaluation of spleen deficiency model: compared with normal mice, the weight of spleen deficiency mice was decreased(P < 0.05), the diet was significantly decreased(P < 0.01), and the anal temperature was decreased(P < 0.05). The body weight of mice in the spleen deficiency HUA group increased gradually during the HUA modeling, and there was no significant difference between the two group at the end of the modeling. The blood uric acid level of mice in spleen deficiency HUA group was higher than that in HUA group(P < 0.05), but there were no significant differences in urea nitrogen and creatinine levels among the four groups. The fecal uric acid of the spleen deficiency HUA group was significantly lower than that of HUA group(P < 0.05). HE staining showed that the villi of ileum and colon tissues were shortened and loosely arranged in the spleen deficiency group, while the villi of jejunum and ileum tissues were loosely arranged in the spleen deficiency HUA group, and goblet cells of colon tissues were reduced. Western Blot analysis showed that the expression of ABCG2 and GLUT9 decreased in colon tissues of spleen deficiency HUA group. IHC analysis showed that the expression of ABCG2 and GLUT9 increased in colon tissues of HUA group compared to blank group, and the expression of ABCG2 and GLUT9 decreased in colon tissues of spleen deficiency HUA group compared to HUA group.Conclusion Intestinal uric acid excretion disorder in hyperuricemia mice with spleen deficiency syndrome leads to increased blood uric acid level, which may be related to the decreased expression of intestinal uric acid transporters ABCG2 and GLUT9.
-
Key words:
- spleen deficiency syndrome /
- hyperuricemia /
- intestinal excretion /
- ABCG2 /
- GLUT9
-

-
[1] Zhang M, Zhu X, Wu J, et al. Prevalence of Hyperuricemia Among Chinese Adults: Findings From Two Nationally Representative Cross-Sectional Surveys in 2015-16 and 2018-19[J]. Front Immunol, 2021, 12(2): 791983.
[2] Tian X, Chen S, Wang P, et al. Temporal relationship between hyperuricemia and hypertension and its impact on future risk of cardiovascular disease[J]. Eur J Intern Med, 2023, 111(5): 82-89.
[3] Wang A, Tian X, Zuo Y, et al. Effect of changes in serum uric acid on the risk of stroke and its subtypes[J]. Nutr Metab Cardiovasc Dis, 2022, 32(1): 167-175. doi: 10.1016/j.numecd.2021.09.017
[4] Xu X, Hu J, Song N, et al. Hyperuricemia increases the risk of acute kidney injury: a systematic review and meta-analysis[J]. BMC Nephrol, 2017, 18(1): 27. doi: 10.1186/s12882-016-0433-1
[5] Yin H, Liu N, Chen J. The Role of the Intestine in the Development ofHyperuricemia[J]. Front Immunol, 2022, 13: 845684. doi: 10.3389/fimmu.2022.845684
[6] Chi X, Zhang H, Zhang S, et al. Chinese herbal medicine for gout: a review of the clinical evidence and pharmacological mechanisms[J]. Chin Med, 2020, 2(12): 15-17.
[7] 尚家驹, 孙淳, 王秀娟, 等. 运脾化浊法治疗脾虚型高尿酸血症回顾性研究[J]. 安徽中医药大学学报, 2021, 40(1): 38-42. https://www.cnki.com.cn/Article/CJFDTOTAL-AHZY202101011.htm
[8] 杨映映, 李青伟, 高泽正, 等. 诸糖脂酸上溢中满皆属于浊——仝小林从浊论治代谢综合征[J]. 吉林中医药, 2018, 38(3): 274-278. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYJL201803008.htm
[9] 谢慧臣, 冉云, 张云, 等. 麸炒苍术对脾虚大鼠结肠组织MEK/ERK信号通路的影响[J]. 中药新药与临床药理, 2023, 34(10): 1363-1369. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYXY202310004.htm
[10] Xiang T, Yang Z, Sun B, et al. Traditional Chinese medicine: Pivotal role of the spleen in the metabolism of aristolochic acid Ⅰ in rats is dependent on oatp2a1[J]. Mol Med Rep, 2016, 14(4): 3243-3250.
[11] 姜泉, 韩曼, 唐晓颇, 等. 痛风和高尿酸血症病证结合诊疗指南[J]. 中医杂志, 2021, 62(14): 1276-1288. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZYZ202114022.htm
[12] Ohashi Y, Toyoda M, Saito N, et al. Evaluation of ABCG2-mediated extra-renal urate excretion in hemodialysis patients[J]. Sci Rep, 2023, 13: 93.
[13] Tin A, Marten J, Halperin Kuhns VL, et al. Target genes, variants, tissues and transcriptional pathways influencing human serum urate levels[J]. Nat Genet, 2019, 51(10): 1459-1474.
[14] Toyoda Y, Mancikova A, Krylov V, et al. Functional Characterization of Clinically-Relevant Rare Variants in ABCG2 Identified in a Gout and Hyperuricemia Cohort[J]. Cell, 2019, 8(4): 363.
[15] Hoque KM, Dixon EE, Lewis RM, et al. The ABCG2 Q141K hyperuricemia and gout associated variant illuminates the physiology of human urate excretion[J]. Nat Commun, 2020, 11(1): 2767.
-




 下载:
下载: