The value of endoscopic features in predicting the risk of ulcers after endoscopic submucosal dissection in patients with early gastric cancer
-
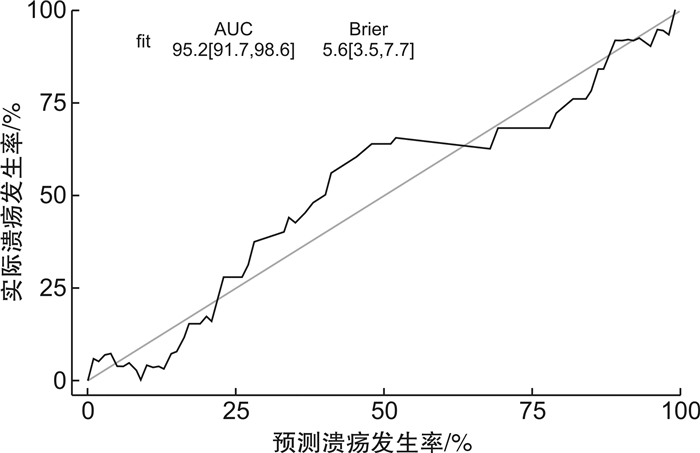
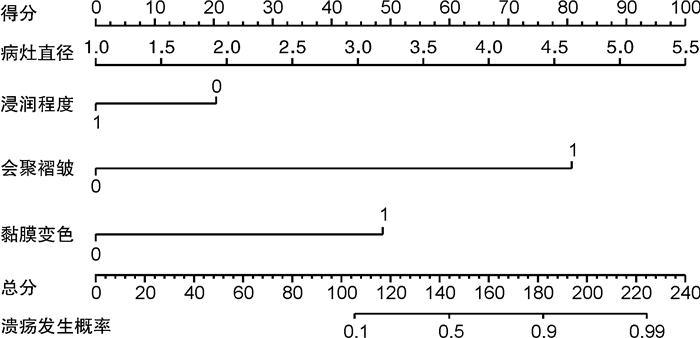
摘要: 目的 探讨内镜特征对早期胃癌患者内镜黏膜下层剥离术(ESD)后溃疡发生风险的预测价值。方法 前瞻性选取2019年1月—2020年5月接受ESD治疗的240例早期胃癌患者为研究对象,随访观察12个月,根据是否发生溃疡分为溃疡组和未发生组。通过多因素分析探求早期胃癌患者ESD术后溃疡发生风险的影响因素,并构建早期胃癌ESD术后溃疡发生风险列线图预测模型,通过一致性指数(C-index指数)检验和绘制校正曲线预测模型效能。结果 截止末次随访时间2021年6月1日,所有患者均获得随访,其中溃疡发生率为17.50%(42/240),无溃疡发生率为82.50%(198/240)。2组病灶直径、会聚褶皱、黏膜变色、浸润深度比较,差异有统计学意义(P< 0.05)。多因素logistic分析显示,病灶直径(OR=3.558,95%CI1.733~7.308),会聚褶皱(OR=100.811,95%CI20.142~504.570),黏膜变色(OR=16.126,95%CI3.213~80.925)为ESD术后溃疡发生的独立危险因素(P< 0.05),浸润深度(OR=0.309,95%CI0.097~0.988)为ESD术后溃疡发生的保护因素(P< 0.05)。基于上述因素的溃疡发生风险预测模型,预测早期胃癌患者ESD术后溃疡发生的C-index为0.952(95%CI0.917~0.986),校正曲线显示实测值与预测值一致性好。结论 病灶直径、会聚褶皱、黏膜变色、浸润深度为早期胃癌患者ESD术后溃疡发生风险的影响因素,基于内镜特征构建的预测模型具有较高的应用价值。Abstract: Objective To explore the value of endoscopic features in predicting the risk of ulcers after endoscopic submucosal dissection(ESD) in patients with early gastric cancer.Methods Atotal of 240 patients with early gastric cancer who received ESD treatment in our hospital from January 2019 to May 2020 were selected as the research objects. The patients were followed up for 12 months, and they were divided into ulcer group and non-occurring group according to whether ulcer occurred. Multi-factor analysis was used to explore the influencing factors of the risk of ulcer after ESD in early gastric cancer patients and construct a nomogram of the risk of ulcer after ESD in early gastric cancer. The model performance was predicted by C-index index test and drawing calibration curve.Results As of the last follow-up time on June 1, 2021, all patients were followed up. Among them, the incidence of ulcers was 17.50%(42/240), and the incidence of non-ulcers was 82.50%(198/240). There were significant differences in lesion diameter, convergent folds, mucosal discoloration, and depth of infiltration between the two groups(P< 0.05). Multivariate logistic analysis showed that lesion diameter(OR=3.558, 95%CI1.733-7.308), convergent folds(OR=100.811, 95%CI20.142-504.570), mucosal discoloration(OR=16.126, 95%CI3.213-80.925) were independent risk factors for ulcers after ESD(P< 0.05), and infiltration depth(OR=0.309, 95%CI0.097-0.988) was a protective factor for ulcers after ESD(P< 0.05). Based on the above factors, the risk prediction model predicted that the consistency index(C-index) of ulcer occurrence after ESD in early gastric cancer patients was 0.952(95%CI0.917-0.986), and the calibration curve showed that the solid-side value was in good agreement with the predicted value.Conclusion The lesion diameter, convergent folds, mucosal discoloration, and depth of infiltration are the influencing factors for the risk of ulcers after ESD in early gastric cancer patients. The prediction model based on endoscopic features has a high application value.
-
Key words:
- early gastric cancer /
- endoscopic submucosal dissection /
- endoscopic features /
- ulcer
-

-
表 1 2组患者一般资料比较
例(%) 一般资料 溃疡组
(42例)未发生组
(198例)t/χ2 P 性别 男 23(54.76) 120(60.61) 0.491 0.483 女 19(45.24) 78(39.39) 年龄/岁 48.96±7.96 49.65± 8.02 0.510 0.612 BMI 22.03±1.52 22.11± 1.48 0.311 0.757 病程/年 2.68±0.86 2.54± 0.79 0.972 0.335 Hp感染史 9(21.43) 32(16.16) 0.679 0.410 胃癌家族史 8(19.05) 26(13.13) 0.997 0.318 病灶直径/cm 4.27±0.74 2.63± 0.65 13.314 < 0.001 病变部位 贲门部 3(7.14) 26(13.13) 胃体部 10(23.81) 53(26.77) 2.648 0.449 胃窦部 22(52.38) 79(39.90) 胃角部 7(16.67) 40(20.20) 肿瘤数量 单发 35(83.33) 172(86.87) 0.365 0.546 多发 7(16.67) 26(13.13) 合并疾病 高血压 12(28.57) 65(32.83) 0.288 0.591 糖尿病 10(23.91) 42(21.21) 0.138 0.711 冠心病 8(19.05) 33(16.67) 0.139 0.710 居住地 农村 28(66.67) 114(57.58) 1.185 0.276 城镇 14(33.33) 84(42.42) 饮酒史 20(47.62) 75(37.88) 1.375 0.241 吸烟史 19(45.24) 82(41.41) 0.208 0.648 表 2 2组内镜特征比较
例(%) 内镜特征 溃疡组
(42例)未发生组
(198例)χ2 P 黏膜变色 是 29(69.05) 65(32.83) 19.078 < 0.001 否 13(30.95) 133(67.17) 会聚褶皱 是 32(76.19) 21(10.61) 83.618 < 0.001 否 10(23.81) 177(89.39) 病变表面情况 凸起 15(35.71) 62(31.32) 平坦 11(26.19) 40(20.20) 1.595 0.450 凹陷 16(38.10) 96(48.48) 黏膜破裂 是 20(47.62) 79(39.90) 0.852 0.356 否 22(52.38) 119(60.10) 浸润深度 黏膜下层 30(71.43) 61(30.81) 24.288 < 0.001 黏膜层 12(28.57) 137(69.19) 表 3 ESD术后溃疡发生风险logistic分析的赋值表
相关因素 变量 赋值 病灶直径 X1 连续变量,实测值 浸润深度 X2 黏膜层=1,黏膜下层=0 会聚褶皱 X3 是=1,否=0 黏膜变色 X4 是=1,否=0 溃疡是否发生 Y 溃疡发生=1,溃疡未发生=0 表 4 ESD术后溃疡发生风险多因素logistic回归分析
相关因素 β SE Wald P OR 95%CI 病灶直径 1.269 0.367 11.949 0.001 3.558 1.733~7.308 浸润深度 -1.173 0.593 3.918 0.048 0.309 0.097~0.988 会聚褶皱 4.613 0.822 31.522 < 0.001 100.811 20.142~504.570 黏膜变色 2.780 0.823 11.413 0.001 16.126 3.213~80.925 常量 -8.306 1.502 30.601 < 0.001 0 -
[1] Barreto SG, Windsor JA. Redefining early gastric cancer[J]. Surg Endosc, 2016, 30(1): 24-37. doi: 10.1007/s00464-015-4184-z
[2] Tao M, Zhou X, Hu M, et al. Endoscopic submucosal dissection versus endoscopic mucosal resection for patients with early gastric cancer: a meta-analysis[J]. BMJ Open, 2019, 9(12): e025803. doi: 10.1136/bmjopen-2018-025803
[3] Hamashima C. Update version of the Japanese Guidelines for Gastric Cancer Screening[J]. Jpn J Clin Oncol, 2018, 48(7): 673-683. doi: 10.1093/jjco/hyy077
[4] Kim Y, Yoon HJ, Kim JH, et al. Effect of histologic differences between biopsy and final resection on treatment outcomes in early gastric cancer[J]. Surg Endosc, 2020, 34(11): 5046-5054. doi: 10.1007/s00464-019-07301-z
[5] Na JE, Lee H, Min YW, et al. Clinical feasibility and oncologic safety of primary endoscopic submucosal dissection for clinical submucosal invasive early gastric cancer[J]. J Cancer Res Clin Oncol, 2021, 147(10): 3051-3061. doi: 10.1007/s00432-021-03581-y
[6] Ono H, Yao K, Fujishiro M, et al. Guidelines for endoscopic submucosal dissection and endoscopic mucosal resection for early gastric cancer[J]. Dig Endosc, 2016, 28(1): 3-15. doi: 10.1111/den.12518
[7] Shimozato A, Sasaki M, Ogasawara N, et al. Risk Factors for Delayed Ulcer Healing after Endoscopic Submucosal Dissection of Gastric Neoplasms[J]. J Gastrointestin Liver Dis, 2017, 26(4): 363-368. doi: 10.15403/jgld.2014.1121.264.kas
[8] 中华医学会消化内镜学分会, 中国抗癌协会肿瘤内镜专业委员会. 中国早期胃癌筛查及内镜诊治共识意见(2014年, 长沙)[J]. 中华消化内镜杂志, 2014, 31(7): 361-377. doi: 10.3760/cma.j.issn.1007-5232.2014.07.001
[9] 所剑. 第5版日本《胃癌治疗指南》更新要点[J]. 中国实用外科杂志, 2017, 37(4): 402-405.
[10] 赵恩昊, 李晓波, 曹晖. 2015年日本消化器内视镜学会《早期胃癌内镜黏膜切除术和黏膜下剥离术治疗指南》解读[J]. 中国实用外科杂志, 2016, 36(1): 79-83.
[11] Mahmoud M, Holzwanger E, Wassef W. Gastric interventional endoscopy[J]. Curr Opin Gastroenterol, 2017, 33(6): 461-466. doi: 10.1097/MOG.0000000000000397
[12] Dohi O, Hatta W, Gotoda T, et al. Long-term outcomes after non-curative endoscopic submucosal dissection for early gastric cancer according to hospital volumes in Japan: a multicenter propensity-matched analysis[J]. Surg Endosc, 2019, 33(12): 4078-4088. doi: 10.1007/s00464-019-06710-4
[13] 刘鑫, 张静, 王晔, 等. 早期胃癌白光内镜下特征分析[J]. 北京大学学报(医学版), 2019, 51(2): 302-306.
[14] Lee YB, Han J, Cho JH, et al. Clinical outcomes of endoscopic surveillance for gastric ulcers in populations with a high prevalence of gastric cancer[J]. Turk J Gastroenterol, 2016, 27(5): 421-427. doi: 10.5152/tjg.2016.16373
[15] Park SM, Kim BW, Kim JS, et al. Can Endoscopic Ulcerations in Early Gastric Cancer Be Clearly Defined before Endoscopic Resection? A Survey among Endoscopists[J]. Clin Endosc, 2017, 50(5): 473-478. doi: 10.5946/ce.2016.143
[16] Shichijo S, Uedo N, Kanesaka T, et al. Long-term outcomes after endoscopic submucosal dissection for differentiated-type early gastric cancer that fulfilled expanded indication criteria: A prospective cohort study[J]. J Gastroenterol Hepatol, 2021, 36(3): 664-670. doi: 10.1111/jgh.15182
[17] Ryu DG, Choi CW, Kang DH, et al. Predictive factors to diagnosis undifferentiated early gastric cancer after endoscopic submucosal dissection[J]. Medicine(Baltimore), 2017, 96(36): e8044.
[18] Kim SJ, Choi CW, Kang DH, et al. Preoperative predictors of beyond endoscopic submucosal dissection indication or lymphovascular invasion in endoscopic resection for early gastric cancer[J]. Surg Endosc, 2018, 32(6): 2948-2957. doi: 10.1007/s00464-017-6009-8
[19] Lee J, Kim BW, Huh CW, et al. Endoscopic Factors that Can Predict Histological Ulcerations in Early Gastric Cancers[J]. Clin Endosc, 2020, 53(3): 328-333. doi: 10.5946/ce.2019.133
[20] Horiuchi Y, Fujisaki J, Yamamoto N, et al. Undifferentiated-type predominant mixed-type early gastric cancer is a significant risk factor for requiring additional surgeries after endoscopic submucosal dissection[J]. Sci Rep, 2020, 10(1): 6748. doi: 10.1038/s41598-020-63781-3
[21] Uzunoglu H, Kaya S. Short-term Prognostic Value of Tumor Diameter in Stage 2 and 3 Gastric Cancer[J]. J Coll Physicians Surg Pak, 2021, 31(3): 288-293. doi: 10.29271/jcpsp.2021.03.288
-




 下载:
下载: