Study on the effect of gastrointestinal three-needle acupuncture combined with Shenling Baizhu powder for the treatment of early enteral nutrition intolerance in critically ill patients
-
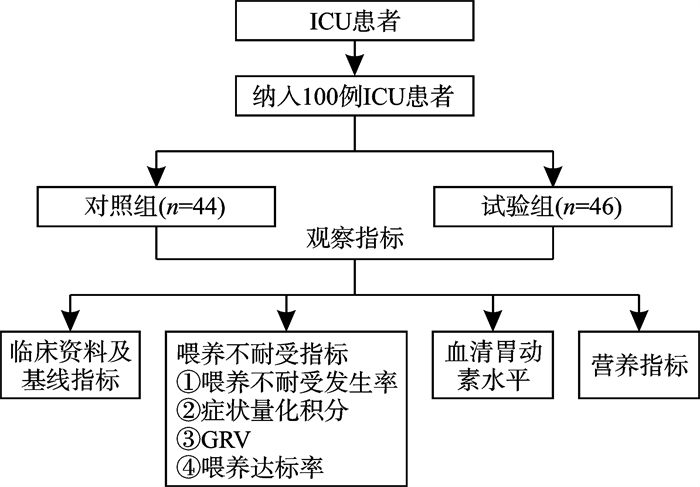
摘要: 目的 探究胃肠三针联合参苓白术散治疗危重症患者早期肠内营养不耐受的效果。方法 纳入100例危重症受试者,随机分为对照组和试验组,对照组采取常规治疗以及对症治疗,试验组采用胃肠三针和参苓白术散联合治疗。干预1周后进行指标检测以及治疗效果评估。结果 治疗后,试验组的喂养不耐受指标分数较对照组明显降低(P < 0.05),血清胃动素水平较对照组明显升高(P < 0.05),营养指标水平变化较对照组更明显(P < 0.05)。结论 胃肠三针联合参苓白术散能够降低危重症患者早期肠内营养不耐受的发生率,联合治疗能够为危重症患者的治疗和康复提供有效支持。Abstract: Objective This study aims to evaluate the efficacy of a combination therapy involving gastrointestinal three-needle acupuncture, Shenling Baizhu powder in reducing early enteral nutrition intolerance among critically ill patients.Methods A total of 100 critically ill patients were randomly assigned to two groups: a control group receiving conventional and symptomatic treatment, and an experimental group receiving a combination of gastrointestinal three-needle acupuncture and Shenling Baizhu powder. After one week of intervention, various indicators were assessed to evaluate the treatment outcomes.Results Post-treatment, the experimental group exhibited a significantly lower feeding intolerance index compared to the control group. Additionally, the serum gastric motility index was significantly higher, and the nutritional index was significantly lower in the experimental group, with statistically significant differences observed between the two groups(P < 0.05).Conclusion The combination of gastrointestinal three-needle acupuncture with Shenling Baizhu powder can effectively reduce the incidence of early enteral nutrition intolerance in critically ill patients. This integrated approach offers valuable support for the treatment and recove.
-

-
表 1 两组患者的临床资料比较
例,X±S 组别 例数 性别 年龄/岁 身高/cm 体重/kg 男 女 对照组 44 20 24 65.46±12.49 168.00±5.99 63.25±10.44 试验组 46 22 24 68.35±15.08 167.85±7.05 68.17±19.08 表 2 两组患者的感染情况及原始疾病比较
例(%) 指标 对照组(n=44) 试验组(n=46) 感染情况 是 30(68.18) 32(69.57) 否 14(31.82) 14(30.43) 脑血管意外 9(20.45) 11(23.91) 肾衰竭 3(6.82) 1(2.17) 心力衰竭 9(20.45) 10(21.74) 呼吸衰竭 6(13.64) 8(17.39) 创伤 8(18.18) 6(13.04) 休克 4(9.09) 3(6.52) 大型手术复苏 2(4.55) 3(6.52) 其他 3(6.82) 4(8.70) 表 3 两组患者的机械通气时间、住院时间、APACHE-Ⅱ评分比较
X±S 组别 例数 机械通气时间/d 住院时间/d APACHE-Ⅱ评分/分 治疗前 治疗后 对照组 44 4.07±1.39 11.80±3.93 16.63±2.86 16.51±3.97 试验组 46 5.76±2.13 11.09±3.52 16.24±4.49 14.00±3.301) 与对照组比较,1)P < 0.05。 表 4 两组患者治疗前后的AGI分级比较
例(%) 组别 例数 治疗前 治疗1周后 Ⅰ级 Ⅱ级 Ⅲ级 Ⅰ级 Ⅱ级 Ⅲ级 对照组 44 10(22.73) 23(52.27) 11(25.00) 23(52.27) 21(47.73) 0 试验组 46 12(26.09) 21(45.65) 12(26.09) 33(71.74)1) 10(21.74)1) 3(6.52)1) 与对照组比较,1)P < 0.05。 表 5 两组患者的EFI、喂养耐受比较
例(%) 组别 例数 EFI 喂养耐受 对照组 44 21(47.73) 25(56.82) 试验组 46 12(26.09)1) 32(69.57) 与对照组比较,1)P < 0.05。 表 6 两组患者的症状量化积分比较
分,X±S 组别 例数 症状量化积分 治疗1 d后 治疗3 d后 治疗7 d后 对照组 44 3.97±1.75 3.14±2.52 3.70±1.61 试验组 46 4.33±2.34 4.27±2.821) 2.05±1.561) 与对照组比较,1)P < 0.05。 表 7 两组患者治疗前后血清胃动素水平比较
ng/L, X±S 组别 例数 治疗前 治疗后 对照组 44 211.74±7.75 241.67±6.59 试验组 46 208.82±10.31 292.49±8.311) 与对照组比较,1)P < 0.05。 表 8 两组患者治疗前后营养指标比较
X±S 营养指标 对照组(44例) 试验组(46例) 治疗前 治疗后 治疗前 治疗后 ALB/(g/L) 29.19±3.37 29.11±3.06 27.44±3.37 34.98±2.411) PA/(mg/L) 125.45±39.78 200.39±84.41 126.97±69.14 267.74±44.751) 与对照组治疗后比较,1)P < 0.05。 -
[1] 周田田, 蒋一诺, 邹圣强. 重症监护室患者肠内营养喂养不耐受的研究进展[J]. 中华灾害救援医学, 2018, 6(11): 656-660.
[2] Blaser AR, Starkopf J, Kirsimägi V, et al. Definition, prevalence, and outcome of feeding intolerance in intensive care: a systematic review and meta-analysis[J]. Acta Anaesthesiol Scand, 2014, 58(8): 914-922. doi: 10.1111/aas.12302
[3] Kreymann KG, Berger MM, Deutz NE, et al. ESPEN Guidelines on Enteral Nutrition: Intensive care[J]. Clin Nutr, 2006, 25(2): 210-223. doi: 10.1016/j.clnu.2006.01.021
[4] Fernández-Ortega JF, Herrero MJ, Martínez GP. Guidelines for specialized nutritional and metabolic support in the critically-ill patient: update. Consensus SEMICYUC-SENPE: indications, timing and routes of nutrient delivery[J]. Nutr Hosp, 2011, 26 Suppl 2: 7-11.
[5] Taylor BE, McClave SA, Martindale RG, et al. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine(SCCM)and American Society for Parenteral and Enteral Nutrition(A.S.P.E.N. )[J]. Crit Care Med, 2016, 44(2): 390-438. doi: 10.1097/CCM.0000000000001525
[6] McClave SA, Gualdoni J, Nagengast A, et al. Gastrointestinal Dysfunction and Feeding Intolerance in Critical Illness: Do We Need an Objective Scoring System?[J]. Curr Gastroenterol Rep, 2020, 22(1): 1. doi: 10.1007/s11894-019-0736-z
[7] Lin J, Liu Y, Ke L, et al. Feeding intolerance score in critically ill patients with enteral nutrition: A post hoc analysis of a prospective study[J]. Nutr Clin Pract, 2022, 37(4): 869-877. doi: 10.1002/ncp.10788
[8] Heyland DK, Ortiz A, Stoppe C, et al. Incidence, Risk Factors, and Clinical Consequence of Enteral Feeding Intolerance in the Mechanically Ventilated Critically Ill: An Analysis of a Multicenter, Multiyear Database[J]. Crit Care Med, 2021, 49(1): 49-59.
[9] Reintam Blaser A, Starkopf J, Alhazzani W, et al. Early enteral nutrition in critically ill patients: ESICM clinical practice guidelines[J]. Intensive Care Med, 2017, 43(3): 380-398. doi: 10.1007/s00134-016-4665-0
[10] Compher C, Bingham AL, McCall M, et al. Guidelines for the provision of nutrition support therapy in the adult critically ill patient: The American Society for Parenteral and Enteral Nutrition[J]. JPEN J Parenter Enteral Nutr, 2022, 46(1): 12-41. doi: 10.1002/jpen.2267
[11] Reintam Blaser A, Malbrain MLNG, Starkopf J, et al. Gastrointestinal function in intensive care patients: terminology, definitions and management. Recommendations of the ESICM Working Group on Abdominal Problems[J]. Intensive Care Med, 2012, 38(3): 384-394. doi: 10.1007/s00134-011-2459-y
[12] 亚洲急危重症协会中国腹腔重症协作组. 重症患者胃肠功能障碍肠内营养专家共识(2021版)[J]. 中华消化外科杂志, 2021, 20(11): 1123-1136.
[13] Hamada SR, Garcon P, Ronot M, et al. Ultrasound assessment of gastric volume in critically ill patients[J]. Intensive Care Med, 2014, 40(7): 965-972. doi: 10.1007/s00134-014-3320-x
[14] 侯锦, 郭爱敏. 床旁超声监测胃残余量应用于重症患者肠内营养的研究进展[J]. 护理学杂志, 2021, 36(2): 101-104.
[15] 熊芳婷, 胡敏, 凌颜, 等. 床旁超声监测胃残余量指导危重症患者早期肠内营养的应用效果[J]. 中国卫生标准管理, 2023, 14(16): 72-76.
[16] 徐晓演, 龚瑜, 吉云兰, 等. 腹内压联合床旁超声监测胃残余量在有创机械通气患者早期肠内营养中的应用[J]. 广西医学, 2023, 45(7): 754-758.
[17] 肖开婷. 胃肠三针改善卒中后胃肠动力障碍的临床疗效观察[D]. 广州: 广州中医药大学, 2019.
[18] Wang K, McIlroy K, Plank LD, et al. Prevalence, Outcomes, and Management of Enteral Tube Feeding Intolerance: A Retrospective Cohort Study in a Tertiary Center[J]. JPEN J Parenter Enteral Nutr, 2017, 41(6): 959-967. doi: 10.1177/0148607115627142
[19] 王春霞, 高培阳, 韩宽怀, 等. 参苓白术散联合肠内营养对危重病患者预后的影响: 多中心随机对照研究[J]. 中国中西医结合杂志, 2020, 40(1): 41-45.
[20] Doig GS, Heighes PT, Simpson F, et al. Early enteral nutrition, provided within 24 h of injury or intensive care unit admission, significantly reduces mortality in critically ill patients: a meta-analysis of randomised controlled trials[J]. Intensive Care Med, 2009, 35(12): 2018-2027. doi: 10.1007/s00134-009-1664-4
[21] Weijs PJ, Looijaard WG, Beishuizen A, et al. Early high protein intake is associated with low mortality and energy overfeeding with high mortality in non-septic mechanically ventilated critically ill patients[J]. Crit Care, 2014, 18(6): 701. doi: 10.1186/s13054-014-0701-z
[22] 郑基和. 胃肠三针调神针法治疗剖宫产术后胃肠功能紊乱的临床疗效观察[D]. 广州: 广州中医药大学, 2021.
[23] 滕彩洪. 胃肠三针在治疗胃肠动力障碍中的应用分析[J]. 世界最新医学信息文摘, 2016, 16(95): 150-152.
[24] 杨德娇, 丘文军. 胃肠三针治疗胃肠动力障碍的临床观察[J]. 中医临床研究, 2016, 8(2): 28-30.
[25] Qin L, Zhang XX, Jin X, et al. The Effect of Acupuncture on Enteral Nutrition and Gastrointestinal Dynamics in Patients Who Have Suffered a Severe Stroke[J]. Curr Neurovasc Res, 2022, 19(3): 275-281. doi: 10.2174/1567202619666220822123023
[26] Ma LY, Liu QQ, Wu L, et al. Effect of electroacupuncture at Zusanli(ST36) and Zhongwan(CV12) on intestinal nutritional feeding intolerance in patients with severe acute pancreatitis[J]. Zhen Ci Yan Jiu, 2021, 46(4): 312-317.
[27] Pfab F, Winhard M, Nowak-Machen M, et al. Acupuncture in Critically Ill Patients Improves Delayed Gastric Emptying[J]. Anesth Analg, 2011, 112(1): 150-155. doi: 10.1213/ANE.0b013e3181fdfac8
[28] 卢广英, 邢训颜, 王嘉昀, 等. 经典名方参苓白术散的研究进展及质量标志物的预测分析[J]. 中国中药杂志, 2022, 47(19): 5171-5181.
[29] Lewis K, Alqahtani Z, Mcintyre L, et al. The efficacy and safety of prokinetic agents in critically ill patients receiving enteral nutrition: a systematic review and meta-analysis of randomized trials[J]. Crit Care, 2016, 20(1): 259. doi: 10.1186/s13054-016-1441-z
[30] 张仲林, 钟玲, 臧志和, 等. 参苓白术散对动物胃肠动力影响的实验研究[J]. 时珍国医国药, 2009, 20(12): 3151-3152.
[31] 陈黎, 蔡敏, 李红. 加减参苓白术散治疗机械通气患者肠内营养不耐受临床观察[J]. 中国中医急症, 2008, 17(12): 1682-1683.
[32] 王丽, 郝海宁, 薛蓉, 等. 经皮穴位电刺激联合参苓白术散在胃肠肿瘤全麻术后患者中的应用效果[J]. 临床医学研究与实践, 2023, 8(3): 115-117.
[33] 郭春花. 针灸联合参苓白术汤治疗晚期大肠癌姑息化疗患者临床观察[J]. 光明中医, 2023, 38(19): 3810-3812.
[34] 杨俊, 郭淋. 泻胃化瘀糊剂对重症脑卒中患者早期肠内营养的影响[J]. 中国中医急症, 2012, 21(11): 1854-1855.
[35] 武书果. 添加四君子汤的肠内营养对危重症患者的免疫功能影响[D]. 广州: 广州中医药大学, 2010.
[36] 孙仁华, 江荣林, 黄曼, 等. 重症患者早期肠内营养临床实践专家共识[J]. 中华危重病急救医学, 2018, 30(8): 715-721.
-

计量
- 文章访问数: 340
- 施引文献: 0



 下载:
下载: