The predictive effect of geriatric nutritional risk index combined with D-dimer on the prognosis of esophageal cancer patients with radiotherapy and chemotherapy
-
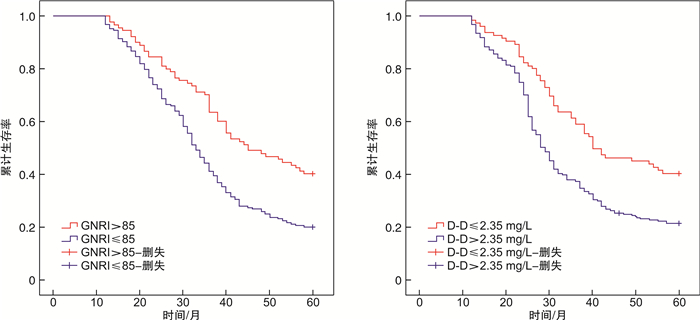
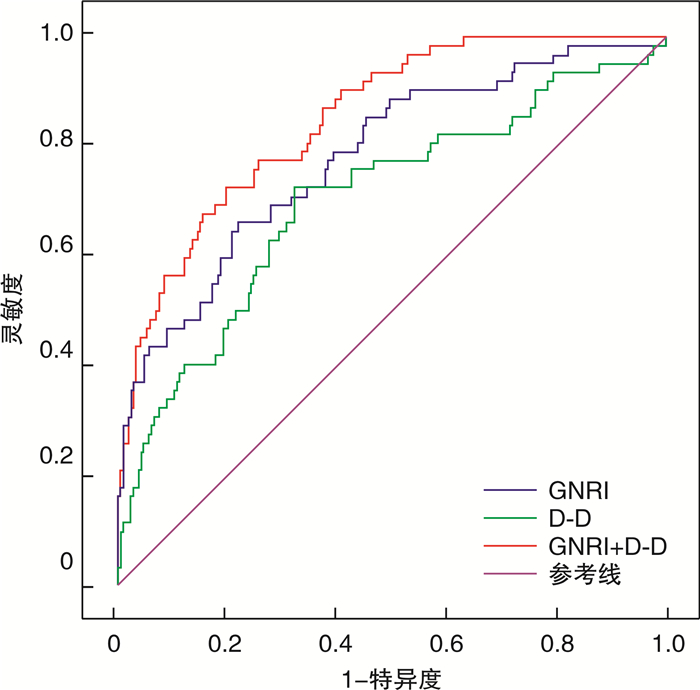
摘要: 目的 探讨老年营养风险指数(GNRI)联合D-二聚体(D-D)在放化疗食管癌患者预后中的预测价值。方法 回顾性分析2016年1月—2019年12月接受根治性放化疗的278例食管癌患者的临床资料,记录患者放化疗前临床资料,并进行随访。采用多因素Cox回归分析食管癌患者死亡的危险因素,并绘制生存曲线图。结果 中位随访时间37个月,278例患者中存活73例(26.26%),死亡205例(73.74%)。受试者工作特征曲线分析显示,GNRI、D-D分别以85、2.35 mg/L预测食管癌死亡的曲线下面积为0.781(95%CI0.714~0.819,P< 0.001)、0.704(95%CI0.625~0.782,P< 0.001),联合预测的曲线下面积为0.851(95%CI0.800~0.819,P=0.901),高于二者单独预测(Z=5.562,P< 0.001;Z=3.816,P< 0.001),且灵敏度和特异度分别为81.95%、78.08%。单因素分析显示,死亡组TNM分期Ⅲ期、低分化、D-D>2.35 mg/L、中性粒细胞/淋巴细胞比值>2.95、GNRI≤85的比例明显高于存活组(P< 0.05)。Kaplan-Meier曲线显示,高GNRI(>85)组生存率(40.00%,36/90)明显高于低GNRI(≤85)组(19.68%,37/188),高D-D(>2.35 mg/L)组生存率(21.88%,42/192)明显低于低D-D(≤2.35 mg/L)组(36.05%,31/86)(P< 0.05)。多因素Cox回归分析结果显示,低分化(HR=1.707,95%CI1.134~2.956,P=0.023)、D-D>2.35 mg/L(HR=1.378,95%CI1.064~2.013,P=0.045)是食管癌患者死亡的独立危险因素,GNRI>85(HR=0.456,95%CI0.137~0.727,P=0.010)为其保护因素。结论 GNRI升高是根治性食管癌患者预后的保护因素,D-D是其危险因素,二者联合检测可精准预测食管癌患者的死亡风险。Abstract: Objective To investigate the predictive value of geriatric nutritional risk index(GNRI) combined with D-dimer(D-D) in the prognosis of patients with esophageal cancer during chemotherapy and radiotherapy.Methods The clinical data of 278 patients with esophageal cancer who received radical radiotherapy and chemotherapy in our hospital from January 2016 to December 2019 were retrospectively analyzed. The clinical data of patients before radiotherapy and chemotherapy were recorded and followed up. Multivariate Cox regression was used to analyze the risk factors of death in patients with esophageal cancer, and the survival curve was drawn.Results The median follow-up time was 37 months. Of the 278 patients, 73 cases(26.26%) survived, and 205 cases(73.74%) died. ROC curve analysis showed that the area under the curve of GNRI and D-D at 85 and 2.35 mg/L to predict esophageal cancer death was 0.781(95%CI0.714-0.819,P< 0.001) and 0.704(95%CI0.625-0.782,P< 0.001), the area under the curve of the combined prediction was 0.851(95%CI0.800-0.819,P=0.901), which was higher than the two independent predictions(Z=5.562,P< 0.001;Z=3.816,P< 0.001), and the sensitivity and the specificity was 81.95% and 78.08% respectively. Univariate analysis showed that the proportions of TNM stage Ⅲ, poorly differentiated, D-D>2.35 mg/L, neutrophil/lymphocyte ratio>2.95, GNRI≤85 in the death group were significantly higher than those in the survival group(P< 0.05). Kaplan-Meier curve showed that the survival rate in the high GNRI(>85) group(40.00%, 36/90) was significantly higher than that in the low GNRI(≤85) group(19.68%, 37/188), and the survival rate in the high D-D(>2.35 mg/L) group(21.88%, 42/192) was lower than that in the low D-D(≤2.35 mg/L) group(36.05%, 31/86)(P< 0.05). The results of multivariate Cox regression analysis showed that poor differentiation(HR=1.707, 95%CI1.134-2.956,P=0.023), D-D>2.35 mg/L(HR=1.378, 95%CI1.064-2.013,P=0.045) were independent risk factors for death in patients with esophageal cancer, and GNRI>85(HR=0.456, 95%CI0.137-0.727,P=0.010) was the protective factor.Conclusion Elevated GNRI is a protective factor for the prognosis of patients with radical esophageal cancer, and D-D is its risk factor. The combined detection of the two indicators can accurately predict the risk of death in patients with esophageal cancer.
-
Key words:
- esophageal cancer /
- radiotherapy /
- chemotherapy /
- geriatric nutritional risk index /
- D-dimer
-

-
表 1 存活组和死亡组临床资料比较
例 临床资料 例数 死亡组
(205例)存活组
(73例)χ2 P 年龄/岁 >70 151 117 34 2.391 0.122 ≤70 127 88 39 性别 男 137 106 31 1.839 0.175 女 141 99 42 高血压 有 96 73 23 0.401 0.527 无 182 132 50 糖尿病 有 58 45 13 0.560 0.454 无 220 160 60 肿瘤部位 食管上段 46 30 16 食管中段 183 138 45 2.068 0.356 食管下段 49 37 12 肿瘤最大径/cm >4 134 102 32 0.756 0.385 ≤4 144 103 41 TNM分期 Ⅰ~Ⅱ期 140 91 49 11.128 0.001 Ⅲ期 138 114 24 分化程度 低分化 68 58 10 6.205 0.013 中高分化 210 147 63 治疗方式 放化疗 62 42 20 1.483 0.223 单纯放疗 216 163 53 CRP/(mg·L-1) >5 135 101 34 0.156 0.693 ≤5 143 104 39 D-D/(mg·L-1) >2.35 187 156 31 27.653 < 0.001 ≤2.35 91 49 42 NLR >2.95 176 138 38 5.398 0.020 ≤2.95 102 67 35 GNRI >85 86 45 41 29.462 < 0.001 ≤85 192 160 32 表 2 食管癌患者死亡危险因素的多因素Cox回归分析结果
危险因素 β SE Wald χ2 HR(95%CI) P TNM分期(Ⅲ期vsⅠ~Ⅱ期) 0.627 0.323 3.768 1.872(0.782~3.153) 0.056 分化程度(低分化vs中高分化) 0.535 0.236 5.139 1.707(1.134~2.956) 0.023 D-D(>2.35 mg/L vs ≤2.35 mg/L) 0.320 0.159 4.050 1.378(1.064~2.013) 0.045 NLR(>2.95 vs
≤2.95)0.269 0.180 2.233 1.309(0.796~2.351) 0.153 GNRI(>85 vs ≤85) -0.786 0.305 6.641 0.456(0.137~0.727) 0.010 -
[1] 陈宏达, 郑荣寿, 王乐, 等. 2019年中国肿瘤流行病学研究进展[J]. 中华疾病控制杂志, 2020, 24(4): 7-13. https://www.cnki.com.cn/Article/CJFDTOTAL-JBKZ202004002.htm
[2] 冯晨曦, 费素娟. 术前纤维蛋白原与前白蛋白比值与食管癌患者病理特征关系及对其诊断价值的研究[J]. 中国中西医结合消化杂志, 2021, 29(10): 725-730. doi: 10.3969/j.issn.1671-038X.2021.10.10
[3] 毛友生, 高树庚, 王群, 等. 中国食管癌临床流行特征及外科治疗概况大数据分析[J]. 中华肿瘤杂志, 2020, 42(3): 228-233. doi: 10.3760/cma.j.cn112152-20191112-00729
[4] Le Bras GF, Farooq MH, Falk GW, et al. Esophageal cancer: The latest on chemoprevention and state of the art therapies[J]. Pharmacol Res, 2016, 113(Pt A): 236-244.
[5] 刘晶晶, 刘漪珊, 朱磊, 等. 302例老年食管癌患者生存时间的影响因素分析[J]. 中国胸心血管外科临床杂志, 2019, 26(1): 89-93. https://www.cnki.com.cn/Article/CJFDTOTAL-ZXYX201901015.htm
[6] 杨冰雪, 程单凤, 潘丽丽, 等. 老年营养风险指数在弥漫大B细胞淋巴瘤患者中的预后意义[J]. 临床血液学杂志, 2018, 31(9): 682-686. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ201809007.htm
[7] 胡思聘, 涂梦芸, 林炜航, 等. 术前老年人营养风险指数对胰腺导管腺癌预后的预测价值[J]. 肝胆胰外科杂志, 2019, 31(5): 271-276. https://www.cnki.com.cn/Article/CJFDTOTAL-GDYW201905005.htm
[8] 舒显竹, 马晓洁. 老年食管癌患者预后营养指数与老年营养风险指数的相关分析[J]. 现代肿瘤医学, 2019, 27(5): 783-786. doi: 10.3969/j.issn.1672-4992.2019.05.017
[9] 李梅, 邱文才, 高琦, 等. 老年营养风险指数在老年胃肠肿瘤围术期的应用[J]. 外科理论与实践, 2021, 26(1): 58-61. https://www.cnki.com.cn/Article/CJFDTOTAL-WKLL202101018.htm
[10] 吴佩纹, 祝淑钗, 宋春洋, 等. 老年营养风险指数对根治性放化疗食管鳞癌患者长期生存的预测价值[J]. 中国肿瘤临床, 2021, 48(14): 721-727. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGZL202114005.htm
[11] 谢恒. 急性白血病患者凝血激活分子的检测及其临床价值[J]. 临床血液学杂志, 2019, 32(4): 268-271. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ201904008.htm
[12] 张廷, 宋腾, 陈馨蕊, 等. D-二聚体水平在初诊弥漫大B细胞淋巴瘤患者预后评估中的价值[J]. 白血病·淋巴瘤, 2021, 30(3): 151-155. doi: 10.3760/cma.j.cn115356-20200803-00195
[13] 曹军丽, 王欣, 郑磊, 等. D-二聚体, 糖类抗原199和胰岛素样生长因子结合蛋白2对可切除胰腺癌患者术后监测和生存期预测的价值[J]. 肿瘤研究与临床, 2020, 32(7): 474-480. doi: 10.3760/cma.j.cn115355-20190808-00349
[14] 屈娜, 王晓彬. D-二聚体和中性粒细胞/淋巴细胞比值评估卵巢癌预后的临床价值[J]. 现代肿瘤医学, 2020, 292(10): 136-141. https://www.cnki.com.cn/Article/CJFDTOTAL-SXZL202010031.htm
[15] 中国医师协会放射肿瘤治疗医师分会, 中华医学会放射肿瘤治疗学分会, 中国抗癌协会肿瘤放射治疗专业委员会. 中国食管癌放射治疗指南(2019年版)[J]. 国际肿瘤学杂志, 2019, 46(7): 385-398. doi: 10.3760/cma.j.issn.1673-422X.2019.07.001
[16] Olivier B, Gilles M, Claire D, et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients[J]. Am J Clin Nutr, 2005, 82(4): 777-783. doi: 10.1093/ajcn/82.4.777
[17] Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012[J]. Int J Cancer, 2015, 136(5): E359-E386. doi: 10.1002/ijc.29210
[18] Faiz Z, Lemmens V, Siersema PD, et al. Increased Resection Rates and Survival Among Patients Aged 75 Years and Older with Esophageal Cancer: A Dutch Nationwide Population-Based Study[J]. World J Surg, 2012, 36(12): 2872-2878. doi: 10.1007/s00268-012-1762-2
[19] 宋春洋, 祝淑钗, 沈文斌, 等. Ⅱ~Ⅲ期食管癌根治性切除术后患者预后的影响因素分析[J]. 天津医药, 2020, 48(3): 55-61. https://www.cnki.com.cn/Article/CJFDTOTAL-TJYZ202003012.htm
[20] 苗晓慧, 尚晓滨, 张洪典, 等. 老年营养风险指数对食管鳞癌患者根治性切除术后生存的影响[J]. 中国肿瘤临床, 2019, 46(6): 33-38. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGZL201906006.htm
[21] Gao ZM, Wang RY, Deng P, et al. TNM-PNI: a novel prognostic scoring system for patients with gastric cancer and curative D2 resection[J]. Cancer Manag Res, 2018, 10: 2925-2933. doi: 10.2147/CMAR.S169206
[22] 唐梦君, 丁叔波, 胡望远. 老年营养风险指数在行放射治疗高龄食管癌患者预后评估中的价值[J]. 中国医药导报, 2020, 536(6): 68-71. https://www.cnki.com.cn/Article/CJFDTOTAL-YYCY202006017.htm
[23] Anandavadivelan P, Lagergren P. Cachexia in patients with oesophageal cancer[J]. Nat Rev Clin Oncol, 2016, 13(3): 185-198. doi: 10.1038/nrclinonc.2015.200
[24] 张翔宇, 杨玉赏, 尚启新, 等. 术前炎症细胞比值与新辅助治疗食管癌患者术后肺炎及远期预后的相关性研究[J]. 中华外科杂志, 2021, 59(8): 660-666. doi: 10.3760/cma.j.cn112139-20210201-00060
[25] Gu WS, Fang WZ, Liu CY, et al. Prognostic significance of combined pretreatment body mass index(BMI)and BMI loss in patients with esophageal cancer[J]. Cancer Manag Res, 2019, 11: 3029-3041. doi: 10.2147/CMAR.S197820
[26] 沙宗美, 鲍扬漪. D-二聚体和肿瘤标记物在胃癌中的诊断价值[J]. 检验医学与临床, 2020, 17(10): 74-77. https://www.cnki.com.cn/Article/CJFDTOTAL-JYYL202010021.htm
[27] 范刚, 张丁兮, 邹燕, 等. 术前血浆D-二聚体水平与早期宫颈癌患者临床病理特征及其预后的相关性[J]. 现代临床医学, 2020, 46(1): 7-10. https://www.cnki.com.cn/Article/CJFDTOTAL-YYCD202001003.htm
[28] 赵乐, 杨国栋, 常永超. D-二聚体联合CA19-9、SCC对食管癌的诊断价值[J]. 实验与检验医学, 2019, 37(5): 882-884. doi: 10.3969/j.issn.1674-1129.2019.05.035
[29] Li J, Zheng Z, Fang M. Impact of pretreatment plasma D-dimer levels and its perioperative change on prognosis in operable esophageal squamous cell carcinoma[J]. Oncotarget, 2017, 8(45): 79537-79545.
[30] 王彦, 李佳龙, 吴砚铭, 等. 术前D-二聚体水平与中国食管癌患者预后关系的系统评价与Meta分析[J]. 中国胸心血管外科临床杂志, 2020, 27(6): 93-96. https://www.cnki.com.cn/Article/CJFDTOTAL-ZXYX202006022.htm
-




 下载:
下载: